Sunday Poster Session
Category: Biliary/Pancreas
P0050 - Utilization of Oral Anticoagulants for Acute Splenic Infarction in the Setting of Pancreatitis: A Systematic Review
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Phong T. Nguyen, MD, MPH, MSN
William Beaumont Army Medical Center
El Paso, TX
Presenting Author(s)
Phong T. Nguyen, MD, MPH, MSN1, Akanksha Togra, MD2, Jose W. Sotelo, MD2, Shivangini Duggal, MD3, Alejandro Robles, MD2, Abhinav Vulisha, MD4
1William Beaumont Army Medical Center, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3TTUHSC, El Paso, TX; 4Texas Tech Health Sciences Center, El Paso, TX
Introduction: Splenic infarction, a complication of pancreatitis, may occur in the setting of increased pro-inflammatory cytokines and systemic vascular injury. This can further predispose to a prothrombotic state and, thus, future thromboembolic events. As of today, there is no consensus on using oral anticoagulants for managing splenic infarction, specifically in the presence of pancreatitis.
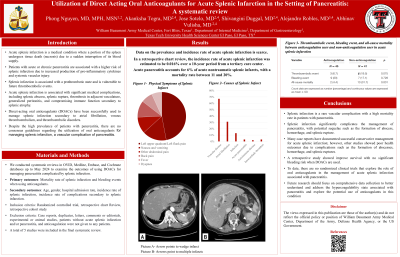
Methods: We conducted systematic reviews in OVID, Medline, Embase, and Cochrane databases up to May 2024 to examine demographic data, hospital admission rates, utilization of oral anticoagulants for management, and health outcomes for patients with pancreatitis complicated by splenic infarction. Data categories included demographics such as age, sex, incidence rate, oral anticoagulants, hospital readmission rate, and mortality rates.
Results: A total of 14 studies were found in the literature search, of which five are retrospective chart reviews/retrospective cohort studies, while others are case reviews and case reports. A retrospective chart review showed that acute splenic infarction is a rare condition from multiple causes, with an incidence rate of 0.016% at an academic hospital over a 10-year period. Incidence of splenic infarct secondary to acute pancreatitis accounts for 6% of all nontraumatic splenic infarct cases. Despite the low incidence, the mortality rate is estimated to be between 11% and 20%. Two epidemiological studies revealed the mean and median age were 57 and 64, respectively. This condition is more common in women, though the sample size in these epidemiological studies was limited. Many case reports have documented successful conservative management for acute splenic infarction; however, other studies showed poor health outcomes due to complications such as the formation of abscesses, hemorrhage, and splenic ruptures. A recent multicenter retrospective cohort study revealed improved survival (HR= 0.06, CI 0.007-0.48, p= 0.008) among anticoagulant users, with no significant difference in the risk of bleeding events (p= 0.728) when compared to anticoagulant non-users.
Discussion: Currently, there are no randomized clinical trials that explore the role of oral anticoagulants in managing acute splenic infarction associated with pancreatitis. Additionally, there is also a lack of data on readmissions. This review highlights the need for more research to be conducted for this indication, including RCTs to explore the role of anticoagulation in splenic infarction and improve patient outcomes.
Disclosures:
Phong T. Nguyen, MD, MPH, MSN1, Akanksha Togra, MD2, Jose W. Sotelo, MD2, Shivangini Duggal, MD3, Alejandro Robles, MD2, Abhinav Vulisha, MD4. P0050 - Utilization of Oral Anticoagulants for Acute Splenic Infarction in the Setting of Pancreatitis: A Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1William Beaumont Army Medical Center, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3TTUHSC, El Paso, TX; 4Texas Tech Health Sciences Center, El Paso, TX
Introduction: Splenic infarction, a complication of pancreatitis, may occur in the setting of increased pro-inflammatory cytokines and systemic vascular injury. This can further predispose to a prothrombotic state and, thus, future thromboembolic events. As of today, there is no consensus on using oral anticoagulants for managing splenic infarction, specifically in the presence of pancreatitis.
Methods: We conducted systematic reviews in OVID, Medline, Embase, and Cochrane databases up to May 2024 to examine demographic data, hospital admission rates, utilization of oral anticoagulants for management, and health outcomes for patients with pancreatitis complicated by splenic infarction. Data categories included demographics such as age, sex, incidence rate, oral anticoagulants, hospital readmission rate, and mortality rates.
Results: A total of 14 studies were found in the literature search, of which five are retrospective chart reviews/retrospective cohort studies, while others are case reviews and case reports. A retrospective chart review showed that acute splenic infarction is a rare condition from multiple causes, with an incidence rate of 0.016% at an academic hospital over a 10-year period. Incidence of splenic infarct secondary to acute pancreatitis accounts for 6% of all nontraumatic splenic infarct cases. Despite the low incidence, the mortality rate is estimated to be between 11% and 20%. Two epidemiological studies revealed the mean and median age were 57 and 64, respectively. This condition is more common in women, though the sample size in these epidemiological studies was limited. Many case reports have documented successful conservative management for acute splenic infarction; however, other studies showed poor health outcomes due to complications such as the formation of abscesses, hemorrhage, and splenic ruptures. A recent multicenter retrospective cohort study revealed improved survival (HR= 0.06, CI 0.007-0.48, p= 0.008) among anticoagulant users, with no significant difference in the risk of bleeding events (p= 0.728) when compared to anticoagulant non-users.
Discussion: Currently, there are no randomized clinical trials that explore the role of oral anticoagulants in managing acute splenic infarction associated with pancreatitis. Additionally, there is also a lack of data on readmissions. This review highlights the need for more research to be conducted for this indication, including RCTs to explore the role of anticoagulation in splenic infarction and improve patient outcomes.
Disclosures:
Phong Nguyen indicated no relevant financial relationships.
Akanksha Togra: Clinexel Inc – Owner/Ownership Interest. Clinexel Life Sciences Pvt Ltd – Owner/Ownership Interest. Cytenet Life science LLP – Owner/Ownership Interest. GLRK Healthcare foundation (Non-profit Organization Company) – Owner/Ownership Interest.
Jose Sotelo indicated no relevant financial relationships.
Shivangini Duggal indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Abhinav Vulisha indicated no relevant financial relationships.
Phong T. Nguyen, MD, MPH, MSN1, Akanksha Togra, MD2, Jose W. Sotelo, MD2, Shivangini Duggal, MD3, Alejandro Robles, MD2, Abhinav Vulisha, MD4. P0050 - Utilization of Oral Anticoagulants for Acute Splenic Infarction in the Setting of Pancreatitis: A Systematic Review, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
