Sunday Poster Session
Category: Biliary/Pancreas
P0056 - Acute Cholangitis In Pancreatic Cancer: Has the Inpatient Prevalence Changed and is it Associated With Worse Outcomes in the Very Elderly?
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Osayande Osagiede, MBBS, MPH
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Osayande Osagiede, MBBS, MPH, Vivek Kumbhari, MBChB, PhD, Frank J. Lukens, MD
Mayo Clinic, Jacksonville, FL
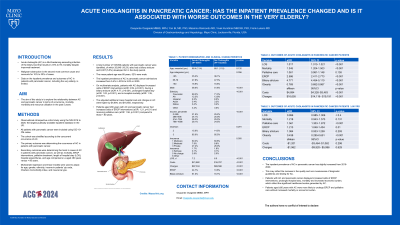
Introduction: Acute cholangitis (AC) is a life-threatening ascending infection of the biliary tract that results in 2.6% to 5% mortality despite improved treatment. Malignant obstruction is the second most common cause and accounts for 10% to 30% of cases. The aim of this study is to explore the relationship between AC and pancreatic cancer in terms of occurrence, mortality, morbidity and resource utilization in the past 5 years.
Methods: Observational retrospective cohort study using the NIS 2016 to 2020, the largest publically available inpatient database in the US. All patients with pancreatic cancer were included using ICD-10-CM codes. The cohort was stratified according to the concurrent occurence of AC. The primary outcome was determining the occurrence of AC in patients with pancreatic cancer. Secondary outcomes were determining the trend in cases of AC in patients with pancreatic cancer, as well as mortality, ERCP interventions, palliative treatment, length of hospital stay (LOS), hospital expenditures, and age comparisons i.e aged ≥80 versus < 80 years.
Results: A total number of 108,690 patients with pancreatic cancer were identified, of which 20,840 (19.2%) also had a biliary stricture and 6,007 (5.5%) developed AC in the study period. The mean patient age was 68 years, 52% were male. The inpatient prevalence of AC in pancreatic cancer admissions increased from 5.4% in 2016 to 5.8% in 2020. Patients with AC displayed increased odds of ERCP interventions (aOR: 2.59, p< 0.001), having a biliary stricture (aOR: 4.77, p< 0.001), prolonged hospital stay (aOR: 1.02, p< 0.001), and in-hospital mortality (aOR: 1.35, p< 0.001). The adjusted additional mean hospital cost and charges in AC were higher by $4,894, and $16,655 respectively. Patients aged ≥80 years with AC and pancreatic cancer had increased odds of ERCP interventions (aOR: 1.21, p=0.01) and receiving palliative care (aOR: 1.56, p< 0.001) compared to those < 80 years.
Discussion: The inpatient prevalence of AC in pancreatic cancer has slightly increased from 2016-2020. This may be a reflection of the increase in the quality and non-invasiveness of diagnostic guidelines and testing for AC. Patients with AC and pancreatic cancer displayed increased odds of ERCP interventions, prolonged hospital stay, mortality and increased economic burden, which reflect the significant healthcare burden generated by AC. Patients aged ≥80 years with AC were more likely to undergo ERCP and palliative care without increased mortality or economic burden.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Osayande Osagiede, MBBS, MPH, Vivek Kumbhari, MBChB, PhD, Frank J. Lukens, MD. P0056 - Acute Cholangitis In Pancreatic Cancer: Has the Inpatient Prevalence Changed and is it Associated With Worse Outcomes in the Very Elderly?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Jacksonville, FL
Introduction: Acute cholangitis (AC) is a life-threatening ascending infection of the biliary tract that results in 2.6% to 5% mortality despite improved treatment. Malignant obstruction is the second most common cause and accounts for 10% to 30% of cases. The aim of this study is to explore the relationship between AC and pancreatic cancer in terms of occurrence, mortality, morbidity and resource utilization in the past 5 years.
Methods: Observational retrospective cohort study using the NIS 2016 to 2020, the largest publically available inpatient database in the US. All patients with pancreatic cancer were included using ICD-10-CM codes. The cohort was stratified according to the concurrent occurence of AC. The primary outcome was determining the occurrence of AC in patients with pancreatic cancer. Secondary outcomes were determining the trend in cases of AC in patients with pancreatic cancer, as well as mortality, ERCP interventions, palliative treatment, length of hospital stay (LOS), hospital expenditures, and age comparisons i.e aged ≥80 versus < 80 years.
Results: A total number of 108,690 patients with pancreatic cancer were identified, of which 20,840 (19.2%) also had a biliary stricture and 6,007 (5.5%) developed AC in the study period. The mean patient age was 68 years, 52% were male. The inpatient prevalence of AC in pancreatic cancer admissions increased from 5.4% in 2016 to 5.8% in 2020. Patients with AC displayed increased odds of ERCP interventions (aOR: 2.59, p< 0.001), having a biliary stricture (aOR: 4.77, p< 0.001), prolonged hospital stay (aOR: 1.02, p< 0.001), and in-hospital mortality (aOR: 1.35, p< 0.001). The adjusted additional mean hospital cost and charges in AC were higher by $4,894, and $16,655 respectively. Patients aged ≥80 years with AC and pancreatic cancer had increased odds of ERCP interventions (aOR: 1.21, p=0.01) and receiving palliative care (aOR: 1.56, p< 0.001) compared to those < 80 years.
Discussion: The inpatient prevalence of AC in pancreatic cancer has slightly increased from 2016-2020. This may be a reflection of the increase in the quality and non-invasiveness of diagnostic guidelines and testing for AC. Patients with AC and pancreatic cancer displayed increased odds of ERCP interventions, prolonged hospital stay, mortality and increased economic burden, which reflect the significant healthcare burden generated by AC. Patients aged ≥80 years with AC were more likely to undergo ERCP and palliative care without increased mortality or economic burden.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Osayande Osagiede indicated no relevant financial relationships.
Vivek Kumbhari: Fujifilm – Consultant. medtronic – Consultant. microtech – Consultant.
Frank J. Lukens indicated no relevant financial relationships.
Osayande Osagiede, MBBS, MPH, Vivek Kumbhari, MBChB, PhD, Frank J. Lukens, MD. P0056 - Acute Cholangitis In Pancreatic Cancer: Has the Inpatient Prevalence Changed and is it Associated With Worse Outcomes in the Very Elderly?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
