Sunday Poster Session
Category: Biliary/Pancreas
P0058 - Congestive Heart Failure Leads to Greater Risk of Developing Post-ERCP Pancreatitis: A Nationwide Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- DA
Daksh Ahluwalia, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Daksh Ahluwalia, MD1, Bhanu Siva Mohan Pinnam, MD1, Mihir P. Shah, MD2, Daniel A. Guifarro, MD1, Abhin Sapkota, MD1, Dushyant S. Dahiya, MD3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 3The University of Kansas School of Medicine, Kansas City, KS
Introduction: Post-Endoscopic Retrograde Cholangiopancreatography (ERCP) pancreatitis (PEP) is the most frequent, dreaded complication of ERCP, leading to significant morbidity in its severe forms. Prevention of PEP is comprised of liberal intravenous hydration, rectally administered nonsteroidal anti-inflammatory drugs, and prophylactic placement of pancreatic duct stents. Management of volume status in patients with congestive heart failure (CHF) is challenging and may lead to an acute exacerbation of CHF. We aimed to investigate the odds of developing PEP in patients with CHF, and inpatient outcomes in this subgroup.
Methods: We utilized the National Inpatient Sample for 2016-2021 to identify all hospitalizations in the United States using the International Classification of Diseases, tenth revision codes in which ERCP was performed, with a tertiary diagnosis of acute pancreatitis. These patients were divided into two groups based on the presence of CHF. Hospitalization characteristics, clinical outcomes, complications, and healthcare burden were compared after adjusting for potential confounders, including myocardial infarction, arrhythmias, carditis, burns, pregnancy.
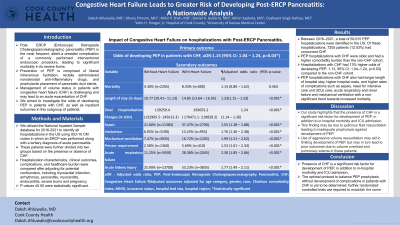
Results: A total of 59,915 PEP hospitalizations were identified, of which 7205 (12.03%) had concurrent CHF. PEP hospitalizations with CHF were older and had a higher comorbidity burden. Hospitalization characteristics between the two groups are compared in Table 1. Hospitalizations with CHF had 13% higher odds of developing PEP [aOR (Adjusted Odds Ratio): 1.13, 95% Confidence Interval (CI): 1.04–1.24, p=0.03], and also had longer length of hospital stay, higher hospital costs, and higher rates of complications such as sepsis, need for intensive care unit (ICU) care, acute renal and respiratory failure, and mechanical ventilation with a non-significant trend towards increased mortality.
Discussion: Our study highlights that the presence of CHF is a significant risk factor for development of PEP, in addition to morbidity and ICU admission. This finding may, in part, be due to judicious fluid resuscitation leading to inadequate prophylaxis against development of PEP. Use of aggressive volume resuscitation may aid in limiting development of PEP but may in turn lead to poor outcomes due to volume overload and pulmonary edema in these patients. The optimal protocol to balance PEP prophylaxis without development of complications in patients with CHF is yet to be determined; randomized controlled trials are required.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Daksh Ahluwalia, MD1, Bhanu Siva Mohan Pinnam, MD1, Mihir P. Shah, MD2, Daniel A. Guifarro, MD1, Abhin Sapkota, MD1, Dushyant S. Dahiya, MD3. P0058 - Congestive Heart Failure Leads to Greater Risk of Developing Post-ERCP Pancreatitis: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2John H. Stroger, Jr. Hospital of Cook County, Cook County, IL; 3The University of Kansas School of Medicine, Kansas City, KS
Introduction: Post-Endoscopic Retrograde Cholangiopancreatography (ERCP) pancreatitis (PEP) is the most frequent, dreaded complication of ERCP, leading to significant morbidity in its severe forms. Prevention of PEP is comprised of liberal intravenous hydration, rectally administered nonsteroidal anti-inflammatory drugs, and prophylactic placement of pancreatic duct stents. Management of volume status in patients with congestive heart failure (CHF) is challenging and may lead to an acute exacerbation of CHF. We aimed to investigate the odds of developing PEP in patients with CHF, and inpatient outcomes in this subgroup.
Methods: We utilized the National Inpatient Sample for 2016-2021 to identify all hospitalizations in the United States using the International Classification of Diseases, tenth revision codes in which ERCP was performed, with a tertiary diagnosis of acute pancreatitis. These patients were divided into two groups based on the presence of CHF. Hospitalization characteristics, clinical outcomes, complications, and healthcare burden were compared after adjusting for potential confounders, including myocardial infarction, arrhythmias, carditis, burns, pregnancy.
Results: A total of 59,915 PEP hospitalizations were identified, of which 7205 (12.03%) had concurrent CHF. PEP hospitalizations with CHF were older and had a higher comorbidity burden. Hospitalization characteristics between the two groups are compared in Table 1. Hospitalizations with CHF had 13% higher odds of developing PEP [aOR (Adjusted Odds Ratio): 1.13, 95% Confidence Interval (CI): 1.04–1.24, p=0.03], and also had longer length of hospital stay, higher hospital costs, and higher rates of complications such as sepsis, need for intensive care unit (ICU) care, acute renal and respiratory failure, and mechanical ventilation with a non-significant trend towards increased mortality.
Discussion: Our study highlights that the presence of CHF is a significant risk factor for development of PEP, in addition to morbidity and ICU admission. This finding may, in part, be due to judicious fluid resuscitation leading to inadequate prophylaxis against development of PEP. Use of aggressive volume resuscitation may aid in limiting development of PEP but may in turn lead to poor outcomes due to volume overload and pulmonary edema in these patients. The optimal protocol to balance PEP prophylaxis without development of complications in patients with CHF is yet to be determined; randomized controlled trials are required.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Daksh Ahluwalia indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Mihir Shah indicated no relevant financial relationships.
Daniel Guifarro indicated no relevant financial relationships.
Abhin Sapkota indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Daksh Ahluwalia, MD1, Bhanu Siva Mohan Pinnam, MD1, Mihir P. Shah, MD2, Daniel A. Guifarro, MD1, Abhin Sapkota, MD1, Dushyant S. Dahiya, MD3. P0058 - Congestive Heart Failure Leads to Greater Risk of Developing Post-ERCP Pancreatitis: A Nationwide Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
