Sunday Poster Session
Category: Biliary/Pancreas
P0003 - Trends and Disparities in Pancreatic Cancer Mortality in the United States From 1999 to 2020
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- HK
Harika Kandlakunta, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Harika Kandlakunta, MD, Liliane Deeb, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Recent data has identified a rise in pancreatic cancer rates with sex and age-related differences in the incidence of pancreatic cancer. It remains unclear if there is a corresponding increase in pancreatic cancer mortality and whether similar demographic differences exist in pancreatic cancer mortality.
Methods: We utilized the Centers for Disease Control and Prevention's Wide‐Ranging Online Data for Epidemiologic Research database (1999-2020) to identify patients aged ≥25 years and with pancreatic cancer as the underlying cause of death. The database uses definitions of World Health Organization to classify underlying cause of death which is defined as the disease or injury that initiates a sequence of events that leads directly to death. Age adjusted mortality rates (AAMR) were calculated per 100,000 individuals standardized to the US census population of the year 2000. Changes in trends of mortality over time were estimated by calculating the annual percentage change (APC) with 95% confidence interval (CI) using the Joinpoint Regression Program.
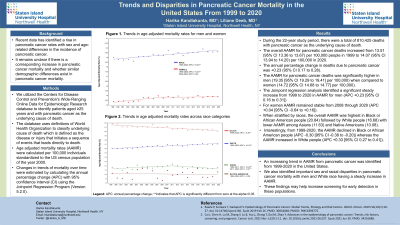
Results: During the 22-year study period, there were a total of 810,425 deaths with pancreatic cancer as the underlying cause of death. The overall AAMR for pancreatic cancer deaths increased from 13.5 (95% CI 13.4 to 13.7) per 100,000 people in 1999 to 14.1 (95% CI 13.9 to 14.2) per 100,000 in 2020. The APC in deaths due to pancreatic cancer was +0.23 (95%CI 0.17 to 0.28). The AAMR for pancreatic cancer deaths was significantly higher in men (19.3 [95% CI 19.3 to 19.4]) when compared to women (14.7 [95% CI 14.7 to 14.8]). The Joinpoint regression analysis identified a steady increase from 1999 to 2020 in AAMR for men (APC +0.23 [95% CI 0.16 to 0.31]); however, for women AAMR remained stable from 2008 through 2020 (APC +0.04 [95% CI -0.64 to +0.16]). When stratified by races, the overall AAMR was highest in Black people (20.84) followed by White people (16.68). Interestingly, from 1999-2020, the AAMR declined in Black people (APC -0.30 [95% CI -0.38 to -0.20]) whereas the AAMR increased in White people (APC +0.33 [95% CI 0.27 to 0.41]).
Discussion: An increasing trend in AAMR for pancreatic cancer was identified from 1999-2020 in the United States. Important sex and racial disparities were identified in pancreatic cancer mortality with men and White race having a steady increase in AAMR. These findings advocate for early screening in these at-risk populations to attain early diagnosis and potentially mitigate the higher mortality rates.
Disclosures:
Harika Kandlakunta, MD, Liliane Deeb, MD. P0003 - Trends and Disparities in Pancreatic Cancer Mortality in the United States From 1999 to 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Recent data has identified a rise in pancreatic cancer rates with sex and age-related differences in the incidence of pancreatic cancer. It remains unclear if there is a corresponding increase in pancreatic cancer mortality and whether similar demographic differences exist in pancreatic cancer mortality.
Methods: We utilized the Centers for Disease Control and Prevention's Wide‐Ranging Online Data for Epidemiologic Research database (1999-2020) to identify patients aged ≥25 years and with pancreatic cancer as the underlying cause of death. The database uses definitions of World Health Organization to classify underlying cause of death which is defined as the disease or injury that initiates a sequence of events that leads directly to death. Age adjusted mortality rates (AAMR) were calculated per 100,000 individuals standardized to the US census population of the year 2000. Changes in trends of mortality over time were estimated by calculating the annual percentage change (APC) with 95% confidence interval (CI) using the Joinpoint Regression Program.
Results: During the 22-year study period, there were a total of 810,425 deaths with pancreatic cancer as the underlying cause of death. The overall AAMR for pancreatic cancer deaths increased from 13.5 (95% CI 13.4 to 13.7) per 100,000 people in 1999 to 14.1 (95% CI 13.9 to 14.2) per 100,000 in 2020. The APC in deaths due to pancreatic cancer was +0.23 (95%CI 0.17 to 0.28). The AAMR for pancreatic cancer deaths was significantly higher in men (19.3 [95% CI 19.3 to 19.4]) when compared to women (14.7 [95% CI 14.7 to 14.8]). The Joinpoint regression analysis identified a steady increase from 1999 to 2020 in AAMR for men (APC +0.23 [95% CI 0.16 to 0.31]); however, for women AAMR remained stable from 2008 through 2020 (APC +0.04 [95% CI -0.64 to +0.16]). When stratified by races, the overall AAMR was highest in Black people (20.84) followed by White people (16.68). Interestingly, from 1999-2020, the AAMR declined in Black people (APC -0.30 [95% CI -0.38 to -0.20]) whereas the AAMR increased in White people (APC +0.33 [95% CI 0.27 to 0.41]).
Discussion: An increasing trend in AAMR for pancreatic cancer was identified from 1999-2020 in the United States. Important sex and racial disparities were identified in pancreatic cancer mortality with men and White race having a steady increase in AAMR. These findings advocate for early screening in these at-risk populations to attain early diagnosis and potentially mitigate the higher mortality rates.
Disclosures:
Harika Kandlakunta indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Harika Kandlakunta, MD, Liliane Deeb, MD. P0003 - Trends and Disparities in Pancreatic Cancer Mortality in the United States From 1999 to 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
