Tuesday Poster Session
Category: Esophagus
P3972 - A Rare Case of Pseudoachalasia Secondary to Mullerian Malignancy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ellen Petryna, MD
Atrium Health
Charlotte, NC
Presenting Author(s)
Ellen Petryna, MD, Jennifer Wellington, DO, MSc
Atrium Health, Charlotte, NC
Introduction: Pseudoachalasia is an esophageal motility disorder in which the radiographic, manometric, and clinical symptoms of achalasia are produced by a secondary etiology. There have been various secondary causes reported; However, in approximately 70% of patients pseudoachalasia is caused by a primary or secondary malignancy (1), and only 6% of cases are caused by a secondary malignancy (2). We report a rare case of pseudoachalasia caused by metastatic Mullerian adenocarcinoma.
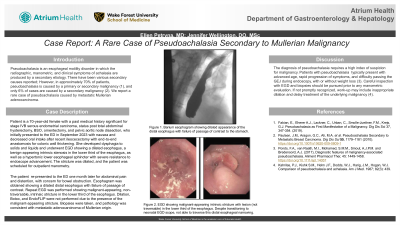
Case Description/Methods: The patient is a 70-year-old female with a past medical history significant for stage IVB serous carcinoma of the endometrium, diagnosed in January 2018, status post total abdominal hysterectomy, bilateral salpingoophorectomy, omentectomy, pelvic aortic node dissection, who initially presented to the ED in September 2023 with nausea and decreased oral intake after recent ileocecectomy with end-to-end anastomosis for colonic wall thickening. She developed dysphagia to both solids and liquids and underwent EGD at an outside hospital showing a dilated upper and middle third of the esophagus, a benign-appearing intrinsic stenosis in the lower third of the esophagus, as well as a hypertonic lower esophageal sphincter with severe resistance to endoscope advancement. The stricture was dilated, and the patient was scheduled for outpatient esophageal manometry. The patient then presented to the ED one month later for abdominal pain and distention, with concern for bowel obstruction. Esophagram was obtained showing a dilated appearance of the distal esophagus with failure of passage of contrast to the stomach. Repeat EGD was performed showing malignant-appearing, non-traversable, intrinsic stricture in the lower third of the esophagus. Dilation, Botox, and EndoFLIP were not performed due to the presence of the malignant-appearing stricture. Biopsies were taken, and pathology was consistent with metastatic adenocarcinoma of Mullerian origin.
Discussion: The diagnosis of pseudoachalasia requires a high index of suspicion for malignancy. Patients with pseudoachalasia typically present with advanced age, rapid progression of symptoms, and difficulty passing the GEJ during endoscopy, with or without weight loss (3). An EGD with biopsies of observed abnormal findings is necessary to establish the correct diagnosis of malignancy-associated pseudoachalasia. If not promptly recognized, work-up may include inappropriate dilation and delay treatment of the underlying malignancy (4).
Disclosures:
Ellen Petryna, MD, Jennifer Wellington, DO, MSc. P3972 - A Rare Case of Pseudoachalasia Secondary to Mullerian Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Atrium Health, Charlotte, NC
Introduction: Pseudoachalasia is an esophageal motility disorder in which the radiographic, manometric, and clinical symptoms of achalasia are produced by a secondary etiology. There have been various secondary causes reported; However, in approximately 70% of patients pseudoachalasia is caused by a primary or secondary malignancy (1), and only 6% of cases are caused by a secondary malignancy (2). We report a rare case of pseudoachalasia caused by metastatic Mullerian adenocarcinoma.
Case Description/Methods: The patient is a 70-year-old female with a past medical history significant for stage IVB serous carcinoma of the endometrium, diagnosed in January 2018, status post total abdominal hysterectomy, bilateral salpingoophorectomy, omentectomy, pelvic aortic node dissection, who initially presented to the ED in September 2023 with nausea and decreased oral intake after recent ileocecectomy with end-to-end anastomosis for colonic wall thickening. She developed dysphagia to both solids and liquids and underwent EGD at an outside hospital showing a dilated upper and middle third of the esophagus, a benign-appearing intrinsic stenosis in the lower third of the esophagus, as well as a hypertonic lower esophageal sphincter with severe resistance to endoscope advancement. The stricture was dilated, and the patient was scheduled for outpatient esophageal manometry. The patient then presented to the ED one month later for abdominal pain and distention, with concern for bowel obstruction. Esophagram was obtained showing a dilated appearance of the distal esophagus with failure of passage of contrast to the stomach. Repeat EGD was performed showing malignant-appearing, non-traversable, intrinsic stricture in the lower third of the esophagus. Dilation, Botox, and EndoFLIP were not performed due to the presence of the malignant-appearing stricture. Biopsies were taken, and pathology was consistent with metastatic adenocarcinoma of Mullerian origin.
Discussion: The diagnosis of pseudoachalasia requires a high index of suspicion for malignancy. Patients with pseudoachalasia typically present with advanced age, rapid progression of symptoms, and difficulty passing the GEJ during endoscopy, with or without weight loss (3). An EGD with biopsies of observed abnormal findings is necessary to establish the correct diagnosis of malignancy-associated pseudoachalasia. If not promptly recognized, work-up may include inappropriate dilation and delay treatment of the underlying malignancy (4).
Disclosures:
Ellen Petryna indicated no relevant financial relationships.
Jennifer Wellington indicated no relevant financial relationships.
Ellen Petryna, MD, Jennifer Wellington, DO, MSc. P3972 - A Rare Case of Pseudoachalasia Secondary to Mullerian Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
