Tuesday Poster Session
Category: Esophagus
P3999 - Enucleating the Imposter: Pseudoachalasia due to a Benign Leiomyoma
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- LL
Lawrence J. Leung, MD, MPH
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Lawrence J. Leung, MD, MPH1, Howard Chang, MD2, Gene K. Ma, MD3, Mitchell Liverant, MD2
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente, Oakland, CA; 3Kaiser Permanente, San Jose, CA
Introduction: Achalasia is a rare esophageal motility disorder characterized by abnormalities in peristalsis and the esophagogastric junction (EGJ) due to idiopathic degeneration of the esophageal myenteric plexus, with an incidence of 1.6 cases per 100,000 people. Pseudoachalasia is an esophageal motility syndrome with symptoms and objective findings indistinguishable from achalasia but arises from a secondary cause that affects the myenteric nerve plexus. It is even more rare, affecting an estimated 1.4-5% of those with achalasia, and commonly due to malignant causes. We present a case of a benign leiomyoma causing symptoms and findings consistent with achalasia subtype II, which was subsequently cured by surgical enucleation.
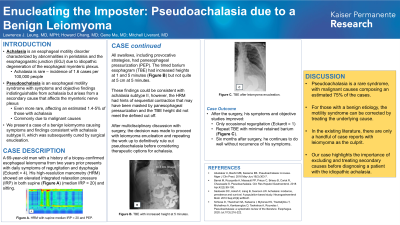
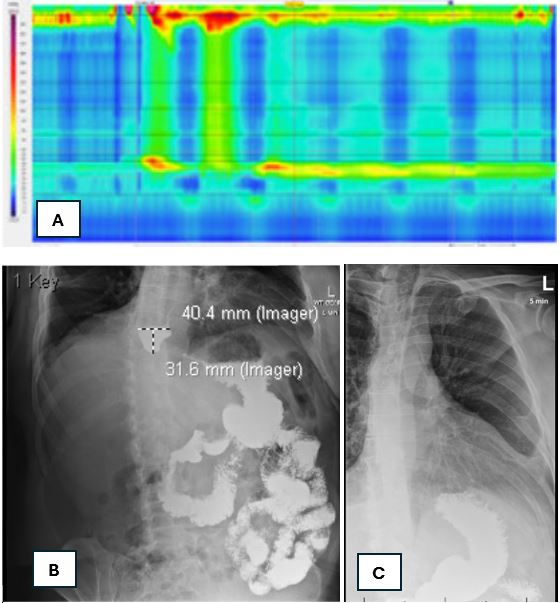
Case Description/Methods: A 69-year-old man with a history of a biopsy-confirmed esophageal leiomyoma from two years prior presents with daily symptoms of regurgitation and dysphagia (Eckardt = 4). His high-resolution manometry (HRM) showed an elevated integrated relaxation pressure (IRP) in both supine (Figure A) and sitting positions. All swallows, including provocative strategies, had panesophageal pressurization. The timed barium esophagram (TBE) had increased heights at 1 and 5 minutes (Figure B) but not quite at 5 cm at 5 minutes. These findings could be consistent with achalasia subtype II, however, the HRM had hints of sequential contraction that may have been masked by panesophageal pressurization and the TBE height did not meet the defined cut off. After multidisciplinary discussion with surgery, the decision was made to proceed with leiomyoma enucleation and repeating the work up to definitively rule out pseudoachalasia before considering therapeutic options for achalasia. After the surgery, his symptoms improved to occasional regurgitation (Eckardt = 1) and his repeat TBE with minimal retained barium (Figure C). Six months later, he continues to do well without recurrence of his symptoms.
Discussion: Pseudoachalasia is a rare syndrome, with malignant causes composing an estimated 75% of the cases. For those with a benign etiology, the motility syndrome can be corrected by treating the underlying cause. In the existing literature, there are only a handful of case reports with leiomyoma as the culprit. Our case highlights the importance of excluding and treating secondary causes before diagnosing a patient with the idiopathic achalasia.
Disclosures:
Lawrence J. Leung, MD, MPH1, Howard Chang, MD2, Gene K. Ma, MD3, Mitchell Liverant, MD2. P3999 - Enucleating the Imposter: Pseudoachalasia due to a Benign Leiomyoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Kaiser Permanente, San Francisco, CA; 2Kaiser Permanente, Oakland, CA; 3Kaiser Permanente, San Jose, CA
Introduction: Achalasia is a rare esophageal motility disorder characterized by abnormalities in peristalsis and the esophagogastric junction (EGJ) due to idiopathic degeneration of the esophageal myenteric plexus, with an incidence of 1.6 cases per 100,000 people. Pseudoachalasia is an esophageal motility syndrome with symptoms and objective findings indistinguishable from achalasia but arises from a secondary cause that affects the myenteric nerve plexus. It is even more rare, affecting an estimated 1.4-5% of those with achalasia, and commonly due to malignant causes. We present a case of a benign leiomyoma causing symptoms and findings consistent with achalasia subtype II, which was subsequently cured by surgical enucleation.
Case Description/Methods: A 69-year-old man with a history of a biopsy-confirmed esophageal leiomyoma from two years prior presents with daily symptoms of regurgitation and dysphagia (Eckardt = 4). His high-resolution manometry (HRM) showed an elevated integrated relaxation pressure (IRP) in both supine (Figure A) and sitting positions. All swallows, including provocative strategies, had panesophageal pressurization. The timed barium esophagram (TBE) had increased heights at 1 and 5 minutes (Figure B) but not quite at 5 cm at 5 minutes. These findings could be consistent with achalasia subtype II, however, the HRM had hints of sequential contraction that may have been masked by panesophageal pressurization and the TBE height did not meet the defined cut off. After multidisciplinary discussion with surgery, the decision was made to proceed with leiomyoma enucleation and repeating the work up to definitively rule out pseudoachalasia before considering therapeutic options for achalasia. After the surgery, his symptoms improved to occasional regurgitation (Eckardt = 1) and his repeat TBE with minimal retained barium (Figure C). Six months later, he continues to do well without recurrence of his symptoms.
Discussion: Pseudoachalasia is a rare syndrome, with malignant causes composing an estimated 75% of the cases. For those with a benign etiology, the motility syndrome can be corrected by treating the underlying cause. In the existing literature, there are only a handful of case reports with leiomyoma as the culprit. Our case highlights the importance of excluding and treating secondary causes before diagnosing a patient with the idiopathic achalasia.
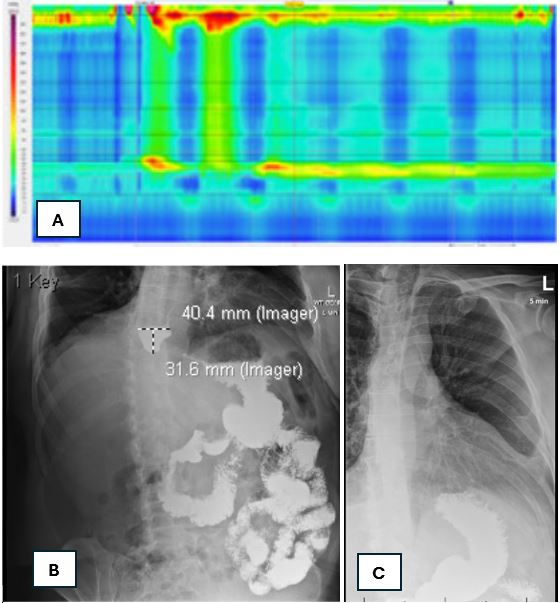
Figure: (A) High-resolution manometry; (B) Timed barium esophagram at 5 minutes; (C) TImed barium esophagram at 5 minutes after surgical enucleation
Disclosures:
Lawrence Leung indicated no relevant financial relationships.
Howard Chang indicated no relevant financial relationships.
Gene Ma indicated no relevant financial relationships.
Mitchell Liverant indicated no relevant financial relationships.
Lawrence J. Leung, MD, MPH1, Howard Chang, MD2, Gene K. Ma, MD3, Mitchell Liverant, MD2. P3999 - Enucleating the Imposter: Pseudoachalasia due to a Benign Leiomyoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
