Tuesday Poster Session
Category: Esophagus
P4007 - Pembrolizumab Associated Acute Esophageal Necrosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Mark Tawfik, DO
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Mark Tawfik, DO1, Elie Bou Sanayeh, MD1, Ahmed Elfiky, MD1, Stephen Mulrooney, MD2
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Mount Sinai South Nassau, Long Island, NY
Introduction: Immune checkpoint inhibitors (ICIs) have revolutionized cancer treatment. They pose
challenges, particularly in the form of immune-related adverse events (irAEs). Although cases of gastrointestinal irAEs have been well-documented, acute esophageal necrosis (AEN) characterized by a circumferential blackening and fragility of the esophagus, weeks after immunotherapy discontinuation, has not been reported.
Case Description/Methods: A 75-year-old diabetic male presented to the GI service with hematemesis. He had recently been diagnosed with high-grade papillary urothelial cancer with liver and retroperitoneal metastases and had undergone radical cystectomy with ileal conduit urinary diversion. He was receiving Pembrolizumab for seven months until it was discontinued three weeks before presentation due to the emergence of grade three immune-mediated colitis.
He presented to the hospital with sepsis secondary to a urinary tract infection, necessitating admission for ceftriaxone treatment and intravenous (IV) fluids administration. On the third day of hospitalization, he experienced hematemesis, with an acute drop in hemoglobin from 10.6 to 5.3 g/L and a rise in serum lactate from 1.5 to 3.6 mmol/L.
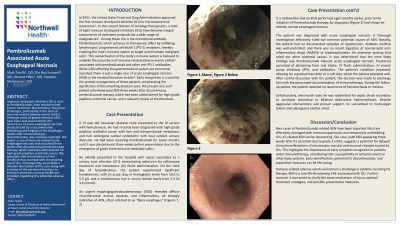
An EGD revealed diffuse circumferential eschar, exudate, and inflammation. (Figures 1)
The patient was diagnosed with AEN. A thorough investigation ruled out common potential causes of AEN. It was determined that the most likely etiology was Pembrolizumab induced AEN. Treatment consisted of bowel rest, IV fluids administration, IV proton pump inhibitors, and antibiotics. The patient's condition improved, allowing for a gradual transition to a soft diet, which the patient tolerated well. The decision was made to discharge him with the permanent discontinuation of immunotherapy. During the follow-up period, he reported no recurrence of hematochezia or melena.
Discussion: Rare cases of Pembrolizumab related AEN have been reported. Most are effectively managed with immunosuppression and temporarily withholding ICIs, ICI-related AEN can be devastating. Our case, with AEN appearing three weeks after ICI cessation due to grade 3 colitis, suggests a potential for delayed clinical manifestations of microscopic vascular and mucosal changes caused by ICIs. This highlights the importance of early symptom recognition in patients under immunotherapy, considering their susceptibility to ischemic events in other body systems. Early identification, potential ICI discontinuation, and supportive measures can be life-saving.

Disclosures:
Mark Tawfik, DO1, Elie Bou Sanayeh, MD1, Ahmed Elfiky, MD1, Stephen Mulrooney, MD2. P4007 - Pembrolizumab Associated Acute Esophageal Necrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Mount Sinai South Nassau, Long Island, NY
Introduction: Immune checkpoint inhibitors (ICIs) have revolutionized cancer treatment. They pose
challenges, particularly in the form of immune-related adverse events (irAEs). Although cases of gastrointestinal irAEs have been well-documented, acute esophageal necrosis (AEN) characterized by a circumferential blackening and fragility of the esophagus, weeks after immunotherapy discontinuation, has not been reported.
Case Description/Methods: A 75-year-old diabetic male presented to the GI service with hematemesis. He had recently been diagnosed with high-grade papillary urothelial cancer with liver and retroperitoneal metastases and had undergone radical cystectomy with ileal conduit urinary diversion. He was receiving Pembrolizumab for seven months until it was discontinued three weeks before presentation due to the emergence of grade three immune-mediated colitis.
He presented to the hospital with sepsis secondary to a urinary tract infection, necessitating admission for ceftriaxone treatment and intravenous (IV) fluids administration. On the third day of hospitalization, he experienced hematemesis, with an acute drop in hemoglobin from 10.6 to 5.3 g/L and a rise in serum lactate from 1.5 to 3.6 mmol/L.
An EGD revealed diffuse circumferential eschar, exudate, and inflammation. (Figures 1)
The patient was diagnosed with AEN. A thorough investigation ruled out common potential causes of AEN. It was determined that the most likely etiology was Pembrolizumab induced AEN. Treatment consisted of bowel rest, IV fluids administration, IV proton pump inhibitors, and antibiotics. The patient's condition improved, allowing for a gradual transition to a soft diet, which the patient tolerated well. The decision was made to discharge him with the permanent discontinuation of immunotherapy. During the follow-up period, he reported no recurrence of hematochezia or melena.
Discussion: Rare cases of Pembrolizumab related AEN have been reported. Most are effectively managed with immunosuppression and temporarily withholding ICIs, ICI-related AEN can be devastating. Our case, with AEN appearing three weeks after ICI cessation due to grade 3 colitis, suggests a potential for delayed clinical manifestations of microscopic vascular and mucosal changes caused by ICIs. This highlights the importance of early symptom recognition in patients under immunotherapy, considering their susceptibility to ischemic events in other body systems. Early identification, potential ICI discontinuation, and supportive measures can be life-saving.

Figure: Figure 1: EGD showing diffuse circumferential eschar, exudate, and inflammation, consistent with Acute Esophageal Necrosis
Disclosures:
Mark Tawfik indicated no relevant financial relationships.
Elie Bou Sanayeh indicated no relevant financial relationships.
Ahmed Elfiky indicated no relevant financial relationships.
Stephen Mulrooney indicated no relevant financial relationships.
Mark Tawfik, DO1, Elie Bou Sanayeh, MD1, Ahmed Elfiky, MD1, Stephen Mulrooney, MD2. P4007 - Pembrolizumab Associated Acute Esophageal Necrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
