Tuesday Poster Session
Category: Esophagus
P4021 - Herniation Two Years After Nissen Fundoplication: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RV
Renuka Verma, MD
University of Nevada
Las Vegas, NV
Presenting Author(s)
Shaunicy Sturm, BS1, Hunter Triplett, BS1, Jacob Austin, DO2, Renuka Verma, MD2, Kamleshun Ramphul, MD3, Ahmad Gill, MD4, Kyaw Min Tun, DO5
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2University of Nevada, Las Vegas, NV; 3Independent Researcher, Triolet, Pamplemousses, Mauritius; 4University of California Davis Medical Center, Sacramento, CA; 5Creighton University School of Medicine, Omaha, NE
Introduction: Nissen fundoplication is an anti-reflux surgical procedure that involves wrapping the gastric fundus around the distal esophagus to reinforce the lower esophageal sphincter. It is recommended for individuals with gastroesophageal reflux disease(GERD) resistant to medical therapy or experiencing recurrent aspiration pneumonia or asthma. However, it carries potential complications, including tissue herniation. Here, we report a case of herniation in a patient with prior Nissen fundoplication, highlighting the critical need to recognize this significant complication.
Case Description/Methods: The patient was a 46-year-old female with a history of irritable bowel syndrome(IBS), cholelithiasis, nonobstructive Schatzki's ring, and GERD who presented to our outpatient clinic post-Nissen fundoplication performed two years ago with dysphagia and non-radiating postprandial right upper quadrant(RUQ) pain that improves with bowel movements. The patient initially agreed to an esophagogastroduodenoscopy (EGD) in five days but presented the next day to the ED with dysphagia, abdominal pain radiating to her back, and vomiting that started six hours after her visit.
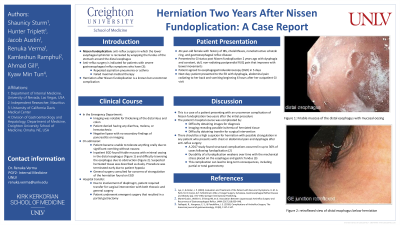
In the ED workup, imaging was notable for thickening of the distal ileum and colon. However, the patient denied having any diarrhea, melena, or hematochezia, and labs demonstrated a negative lipase. After admission, the patient became unable to tolerate anything orally due to vomiting. An inpatient EGD found friable mucosa with oozing in the distal esophagus and difficulty traversing the esophagus due to obstruction (Figure 1). The report included a suspected herniation with dusky tissue. Due to the involvement of the diaphragm, the patient required transfer for surgical intervention with both thoracic and general surgery, and she eventually underwent emergent surgery that resulted in a partial gastrectomy.
Discussion: This case illustrates a complication of Nissen fundoplication, occurring two years post-surgery. Challenges included diagnostic imaging, tissue ischemia, and complicated surgical intervention. Patients with post-fundoplication chest or abdominal pain and dysphagia warrant suspicion of herniation with potential strangulation, as structural complications affect up to 30% of cases. Long-term consequences, such as partial or total gastrectomy, emphasize the importance of early recognition and intervention for this complication.

Disclosures:
Shaunicy Sturm, BS1, Hunter Triplett, BS1, Jacob Austin, DO2, Renuka Verma, MD2, Kamleshun Ramphul, MD3, Ahmad Gill, MD4, Kyaw Min Tun, DO5. P4021 - Herniation Two Years After Nissen Fundoplication: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV; 2University of Nevada, Las Vegas, NV; 3Independent Researcher, Triolet, Pamplemousses, Mauritius; 4University of California Davis Medical Center, Sacramento, CA; 5Creighton University School of Medicine, Omaha, NE
Introduction: Nissen fundoplication is an anti-reflux surgical procedure that involves wrapping the gastric fundus around the distal esophagus to reinforce the lower esophageal sphincter. It is recommended for individuals with gastroesophageal reflux disease(GERD) resistant to medical therapy or experiencing recurrent aspiration pneumonia or asthma. However, it carries potential complications, including tissue herniation. Here, we report a case of herniation in a patient with prior Nissen fundoplication, highlighting the critical need to recognize this significant complication.
Case Description/Methods: The patient was a 46-year-old female with a history of irritable bowel syndrome(IBS), cholelithiasis, nonobstructive Schatzki's ring, and GERD who presented to our outpatient clinic post-Nissen fundoplication performed two years ago with dysphagia and non-radiating postprandial right upper quadrant(RUQ) pain that improves with bowel movements. The patient initially agreed to an esophagogastroduodenoscopy (EGD) in five days but presented the next day to the ED with dysphagia, abdominal pain radiating to her back, and vomiting that started six hours after her visit.
In the ED workup, imaging was notable for thickening of the distal ileum and colon. However, the patient denied having any diarrhea, melena, or hematochezia, and labs demonstrated a negative lipase. After admission, the patient became unable to tolerate anything orally due to vomiting. An inpatient EGD found friable mucosa with oozing in the distal esophagus and difficulty traversing the esophagus due to obstruction (Figure 1). The report included a suspected herniation with dusky tissue. Due to the involvement of the diaphragm, the patient required transfer for surgical intervention with both thoracic and general surgery, and she eventually underwent emergent surgery that resulted in a partial gastrectomy.
Discussion: This case illustrates a complication of Nissen fundoplication, occurring two years post-surgery. Challenges included diagnostic imaging, tissue ischemia, and complicated surgical intervention. Patients with post-fundoplication chest or abdominal pain and dysphagia warrant suspicion of herniation with potential strangulation, as structural complications affect up to 30% of cases. Long-term consequences, such as partial or total gastrectomy, emphasize the importance of early recognition and intervention for this complication.

Figure: Figure 1: Top picture: Friable mucosa of the distal esophagus with mucosal oozing
Bottom picture: retroflexed view of distal esophagus below herniation
Bottom picture: retroflexed view of distal esophagus below herniation
Disclosures:
Shaunicy Sturm indicated no relevant financial relationships.
Hunter Triplett indicated no relevant financial relationships.
Jacob Austin indicated no relevant financial relationships.
Renuka Verma indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Ahmad Gill indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Shaunicy Sturm, BS1, Hunter Triplett, BS1, Jacob Austin, DO2, Renuka Verma, MD2, Kamleshun Ramphul, MD3, Ahmad Gill, MD4, Kyaw Min Tun, DO5. P4021 - Herniation Two Years After Nissen Fundoplication: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
