Tuesday Poster Session
Category: Esophagus
P4024 - An Incidental Finding of Esophageal Epidermoid Metaplasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Elise Le Cam, MD
Banner - University of Arizona
Tucson, AZ
Presenting Author(s)
Elise Le Cam, MD1, Rodrigo Alvarez, DO1, Joseph Kim, MD1, Shivanand Bomman, MD1, Samuel H. Cheong, DO1, Erica Worswick, MD1, Avin Aggarwal, MD2
1Banner - University of Arizona, Tucson, AZ; 2University of Arizona, Tucson, AZ
Introduction:
Esophageal epidermoid metaplasia is a rare condition, most often found in the mid to distal aspect of the esophagus, that can often be mistaken for esophageal leukoplakia (1). Pathophysiology is thought to be related to chemical or mechanical irritation, as it is commonly seen in patients with GERD, alcohol abuse or tobacco use (2).
Case Description/Methods:
A 66-year-old female presented for further evaluation of her refractory GERD and bloating. The patient reported longstanding reflux with occasional associated regurgitation for which she previously tried multiple proton pump inhibitors (PPIs) with minimal benefits. An EGD was performed 2 years earlier with no esophageal plaques identified at that time.
With worsening symptoms of GERD, a repeat EGD was performed. A single plaque with abnormal mucosa and raised margins was found in the middle third of the esophagus at 26 cm measuring approximately 3 cm in largest dimension. The plaque was biopsied and the patient tolerated the procedure well. Histopathology examination confirmed squamous mucosa with benign epidermoid metaplasia. No dysplasia or carcinoma was noted.
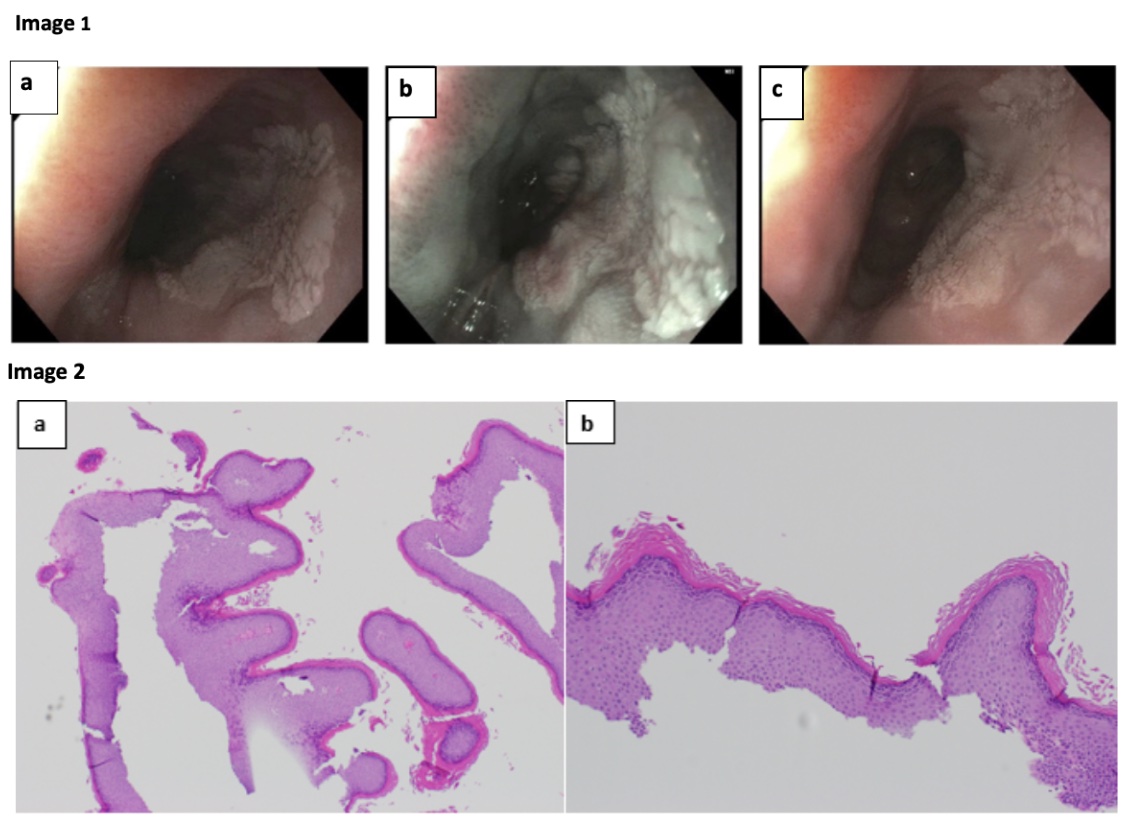
Discussion: Epidermoid metaplasia is defined histologically by the presence of a dense granular layer with overlying hyperorthokeratosis in the squamous mucosa of the esophagus (2). Endoscopically, a white flat to nodular plaque is visualized (3). These lesions may range from small and focal to diffuse and pan-esophageal lesions (3).
The underlying etiology of epidermoid metaplasia remains unclear but smoking and alcohol have been recognized as contributing risk factors (3). An association between epidermoid metaplasia and squamous dysplasia and carcinoma has been reported although the evidence is still limited (3). Either endoscopic ablation or close surveillance has been recommended, with surveillance EGD recommended within the first 6 months after diagnosis and then yearly if no dysplasia is noted (3). This case highlights the importance of close examination of the esophagus for less common lesions that could potentially have severe consequences, if missed.
References:
Disclosures:
Elise Le Cam, MD1, Rodrigo Alvarez, DO1, Joseph Kim, MD1, Shivanand Bomman, MD1, Samuel H. Cheong, DO1, Erica Worswick, MD1, Avin Aggarwal, MD2. P4024 - An Incidental Finding of Esophageal Epidermoid Metaplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Banner - University of Arizona, Tucson, AZ; 2University of Arizona, Tucson, AZ
Introduction:
Esophageal epidermoid metaplasia is a rare condition, most often found in the mid to distal aspect of the esophagus, that can often be mistaken for esophageal leukoplakia (1). Pathophysiology is thought to be related to chemical or mechanical irritation, as it is commonly seen in patients with GERD, alcohol abuse or tobacco use (2).
Case Description/Methods:
A 66-year-old female presented for further evaluation of her refractory GERD and bloating. The patient reported longstanding reflux with occasional associated regurgitation for which she previously tried multiple proton pump inhibitors (PPIs) with minimal benefits. An EGD was performed 2 years earlier with no esophageal plaques identified at that time.
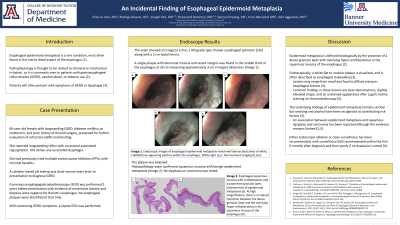
With worsening symptoms of GERD, a repeat EGD was performed. A single plaque with abnormal mucosa and raised margins was found in the middle third of the esophagus at 26 cm measuring approximately 3 cm in largest dimension. The plaque was biopsied and the patient tolerated the procedure well. Histopathology examination confirmed squamous mucosa with benign epidermoid metaplasia. No dysplasia or carcinoma was noted.
Discussion: Epidermoid metaplasia is defined histologically by the presence of a dense granular layer with overlying hyperorthokeratosis in the squamous mucosa of the esophagus (2). Endoscopically, a white flat to nodular plaque is visualized (3). These lesions may range from small and focal to diffuse and pan-esophageal lesions (3).
The underlying etiology of epidermoid metaplasia remains unclear but smoking and alcohol have been recognized as contributing risk factors (3). An association between epidermoid metaplasia and squamous dysplasia and carcinoma has been reported although the evidence is still limited (3). Either endoscopic ablation or close surveillance has been recommended, with surveillance EGD recommended within the first 6 months after diagnosis and then yearly if no dysplasia is noted (3). This case highlights the importance of close examination of the esophagus for less common lesions that could potentially have severe consequences, if missed.
References:
- Gosnell HL, et al. Esophageal Epidermoid Metaplasia: Skin in the Game. 2021;19(5):e46.
- Cottreau J, et al. Prevalence of oesophageal epidermoid metaplasia in 1048 consecutive patients and 58 patients with squamous neoplasms. 2016;68(7):988-995.
- Singhi AD, et al. Esophageal leukoplakia or epidermoid metaplasia: a clinicopathological study of 18 patients. 2014;27(1):38-43.
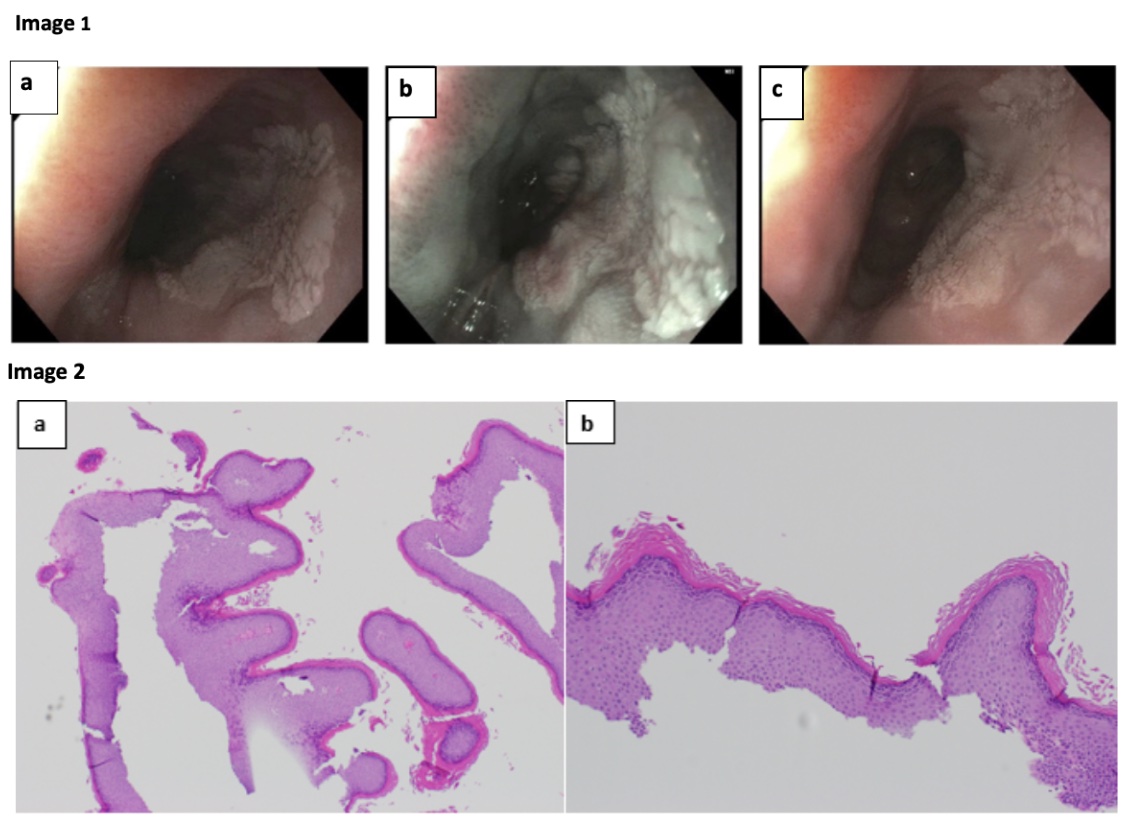
Figure: Image 1: Endoscopic images of esophageal epidermoid metaplasia reveal well demarcated areas of white, cobblestone-appearing patches within the esophagus. White light (a, c). Narrow band imaging (b).
Image 2: Esophageal squamous mucosa with orthokeratosis and a prominent granular layer, characteristic of epidermoid metaplasia (a). At high magnification, there is an abrupt transition between the dense granular layer and the overlying hyperorthokeratosis in the squamous mucosa of the esophagus (b).
Image 2: Esophageal squamous mucosa with orthokeratosis and a prominent granular layer, characteristic of epidermoid metaplasia (a). At high magnification, there is an abrupt transition between the dense granular layer and the overlying hyperorthokeratosis in the squamous mucosa of the esophagus (b).
Disclosures:
Elise Le Cam indicated no relevant financial relationships.
Rodrigo Alvarez indicated no relevant financial relationships.
Joseph Kim indicated no relevant financial relationships.
Shivanand Bomman indicated no relevant financial relationships.
Samuel Cheong indicated no relevant financial relationships.
Erica Worswick indicated no relevant financial relationships.
Avin Aggarwal indicated no relevant financial relationships.
Elise Le Cam, MD1, Rodrigo Alvarez, DO1, Joseph Kim, MD1, Shivanand Bomman, MD1, Samuel H. Cheong, DO1, Erica Worswick, MD1, Avin Aggarwal, MD2. P4024 - An Incidental Finding of Esophageal Epidermoid Metaplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
