Tuesday Poster Session
Category: Esophagus
P4027 - Acute Eosinophilic Appendicitis (AEA) Unmasking Eosinophilic Gastrointestinal Disorder (EGID) in a Misdiagnosed Case!
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ruchir Damjibhai Paladiya, MBBS
University of Connecticut Health Center
Hartford, CT
Presenting Author(s)
Ruchir Damjibhai. Paladiya, MBBS1, Houman Rezaizadeh, MD2
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health Center, Farmington, CT
Introduction: Eosinophilic Gastrointestinal Disorders (EGIDs) are chronic, progressive, immune-mediated disorders with pathologic eosinophilic infiltration in specific regions of gastrointestinal tract along with clinical symptoms in the absence of secondary causes of eosinophilia. We present a case of Acute Eosinophilic Appendicitis (AEA) as an initial presentation in a patient mislabeled to have Irritable Bowel Syndrome-Diarrhea (IBS-D) who was later found to have EGID.
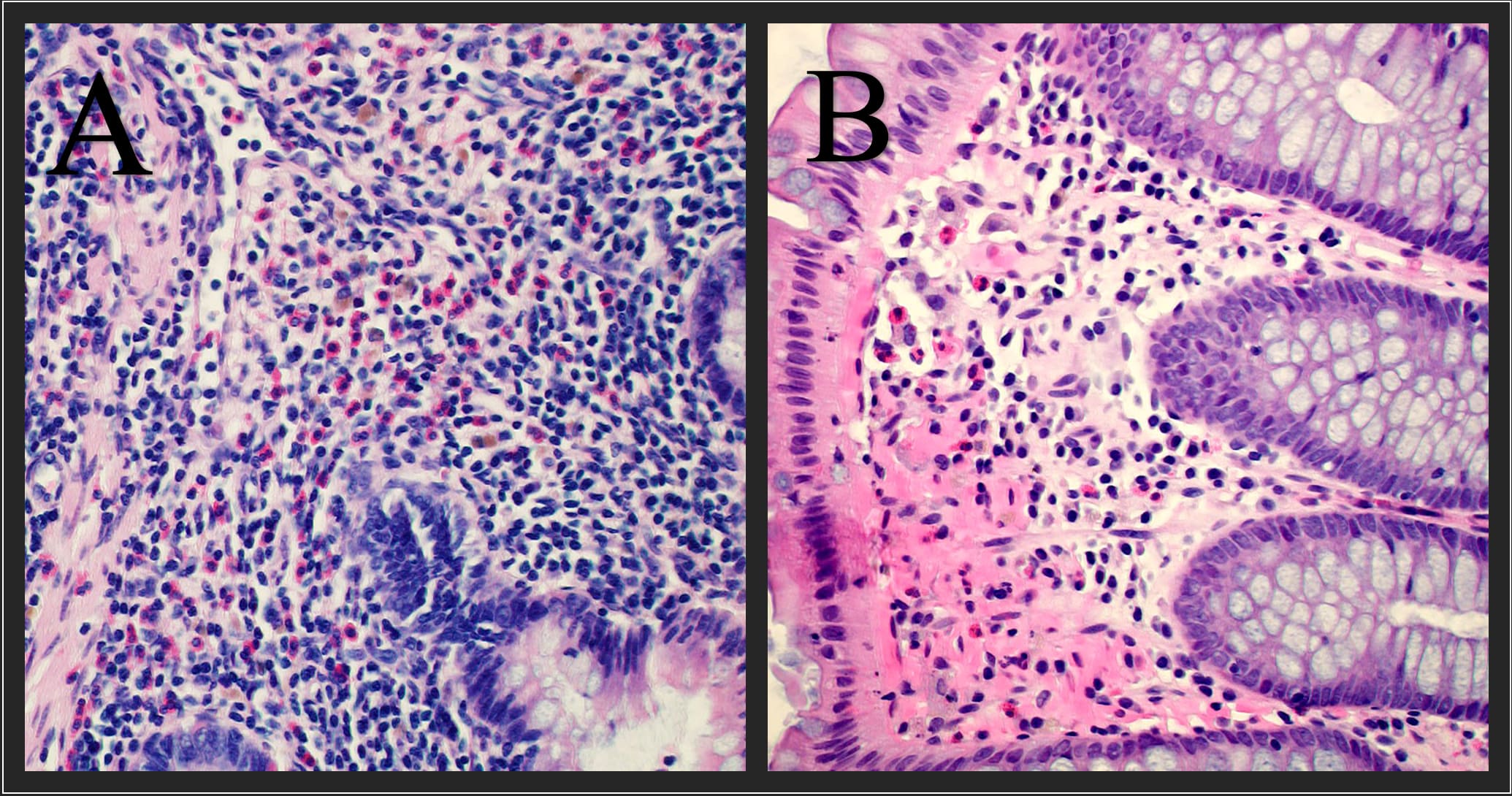
Case Description/Methods: A 35 yo female with PMHx of seasonal allergies, childhood asthma, and IBS-D presented to the ED with acute RLQ abdominal pain. Vital signs were unremarkable. Laboratory tests showed mild leucocytosis 11.4 10*3/uL and CT showed acute appendicitis necessitating laparoscopic appendectomy. Pathology showed appendiceal mucosa with innumerable eosinophils >100/hpf without evidence of neutrophilic appendicitis (Figure 1a). After discharge in the GI clinic she reported a 6 year h/o of dyspepsia, intermittent abdominal pain\cramping in varying quadrants, and fecal urgency with 4 loose, non-bloody BMs daily. Years prior she was diagnosed with IBS-D, had a prior EGD, colonoscopy and multiple CT’s which were unremarkable. She has tried rifaximin and IBGard for her IBS without success. Lab evaluation showed normal Celiac panel, stool cultures, O&P, C. diff, strongyloides IgG, toxocara IgG, campylobacter culture, peripheral smear, flow cytometry, tryptase, CRP, immunoglobulins, HIV and iron studies. Endoscopy with numerous biopsies showed eosinophilic infiltrates in stomach (8/hpf), duodenum (27/hpf), esophagus (< 1/hpf), ileum (25/hpf) and colon (30/hpf) (Figure 1b). Despite these numbers not meeting cut-off criteria for EGIDs, due to on-going symptoms impact on quality of life, prednisone taper starting at 20 mg daily was started. She noted drastic improvement with complete resolution of her GI symptoms further supporting our suspicion of an underlying EGID.
Discussion: Our patient's initial presentation of AEA (an EGID-associated complication) and steroid responsiveness pointed towards EGID as the main etiology of her symptoms previously misdiagnosed as IBS-D. It is possible that EGID criteria on pathology were not met due to the patchy nature of the disease. This novel finding does point towards the potential need for re-evaluating the cut-off criteria for EGIDs as well as having a high index of suspicion for EGIDs in patients with atopy. It also highlights the necessity for a standardized biopsy protocol for each EGID organ.
Disclosures:
Ruchir Damjibhai. Paladiya, MBBS1, Houman Rezaizadeh, MD2. P4027 - Acute Eosinophilic Appendicitis (AEA) Unmasking Eosinophilic Gastrointestinal Disorder (EGID) in a Misdiagnosed Case!, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Hartford, CT; 2University of Connecticut Health Center, Farmington, CT
Introduction: Eosinophilic Gastrointestinal Disorders (EGIDs) are chronic, progressive, immune-mediated disorders with pathologic eosinophilic infiltration in specific regions of gastrointestinal tract along with clinical symptoms in the absence of secondary causes of eosinophilia. We present a case of Acute Eosinophilic Appendicitis (AEA) as an initial presentation in a patient mislabeled to have Irritable Bowel Syndrome-Diarrhea (IBS-D) who was later found to have EGID.
Case Description/Methods: A 35 yo female with PMHx of seasonal allergies, childhood asthma, and IBS-D presented to the ED with acute RLQ abdominal pain. Vital signs were unremarkable. Laboratory tests showed mild leucocytosis 11.4 10*3/uL and CT showed acute appendicitis necessitating laparoscopic appendectomy. Pathology showed appendiceal mucosa with innumerable eosinophils >100/hpf without evidence of neutrophilic appendicitis (Figure 1a). After discharge in the GI clinic she reported a 6 year h/o of dyspepsia, intermittent abdominal pain\cramping in varying quadrants, and fecal urgency with 4 loose, non-bloody BMs daily. Years prior she was diagnosed with IBS-D, had a prior EGD, colonoscopy and multiple CT’s which were unremarkable. She has tried rifaximin and IBGard for her IBS without success. Lab evaluation showed normal Celiac panel, stool cultures, O&P, C. diff, strongyloides IgG, toxocara IgG, campylobacter culture, peripheral smear, flow cytometry, tryptase, CRP, immunoglobulins, HIV and iron studies. Endoscopy with numerous biopsies showed eosinophilic infiltrates in stomach (8/hpf), duodenum (27/hpf), esophagus (< 1/hpf), ileum (25/hpf) and colon (30/hpf) (Figure 1b). Despite these numbers not meeting cut-off criteria for EGIDs, due to on-going symptoms impact on quality of life, prednisone taper starting at 20 mg daily was started. She noted drastic improvement with complete resolution of her GI symptoms further supporting our suspicion of an underlying EGID.
Discussion: Our patient's initial presentation of AEA (an EGID-associated complication) and steroid responsiveness pointed towards EGID as the main etiology of her symptoms previously misdiagnosed as IBS-D. It is possible that EGID criteria on pathology were not met due to the patchy nature of the disease. This novel finding does point towards the potential need for re-evaluating the cut-off criteria for EGIDs as well as having a high index of suspicion for EGIDs in patients with atopy. It also highlights the necessity for a standardized biopsy protocol for each EGID organ.
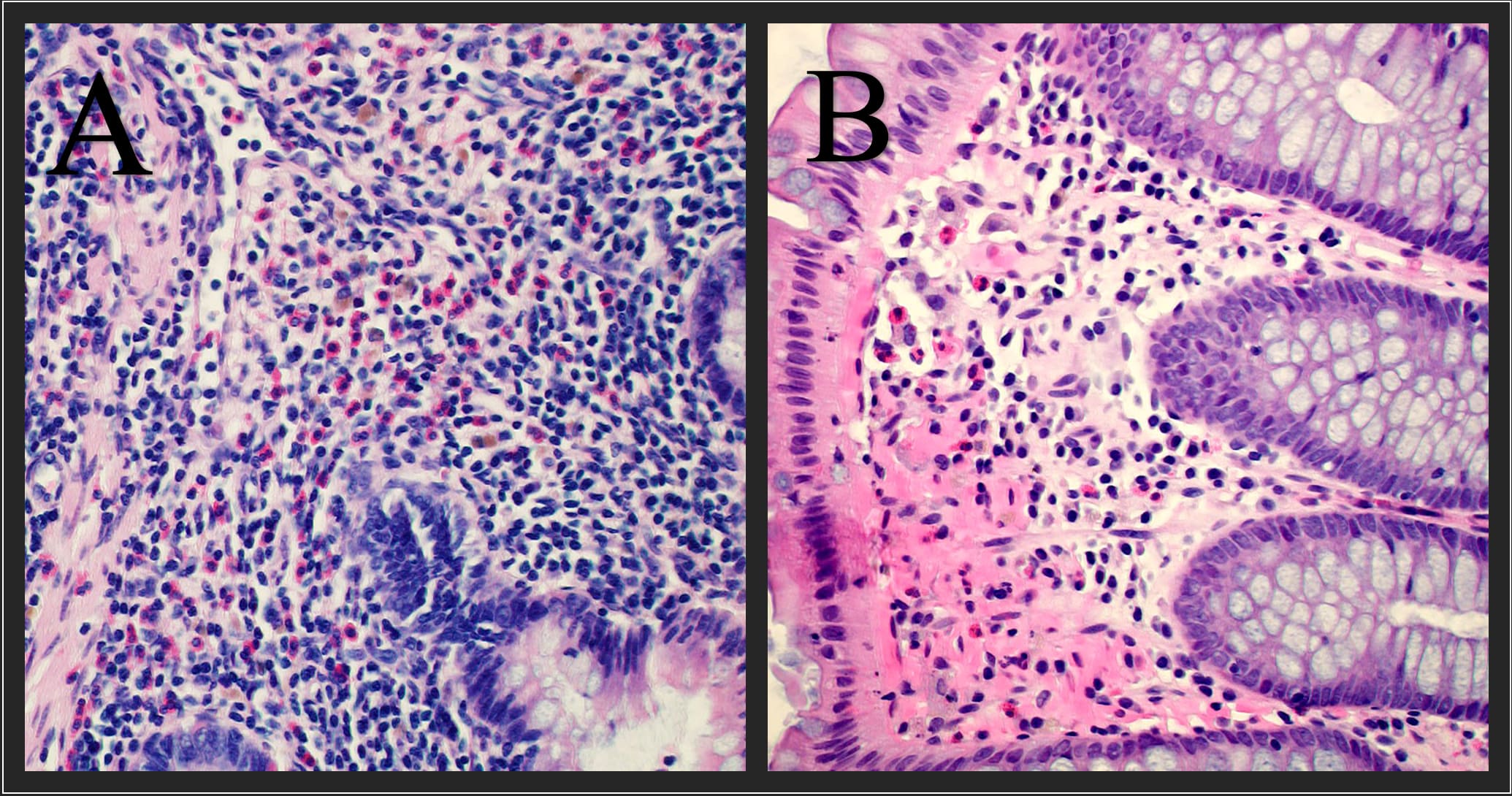
Figure: Figure 1A. Appendix with abundant eosinophilic infiltrates. Overall study reported up to >100 eosinophils/hpf.
Figure 1B. Colonic mucosa with mild eosinophilia. Overall study reported up to 20 eosinophils/hpf.
Figure 1B. Colonic mucosa with mild eosinophilia. Overall study reported up to 20 eosinophils/hpf.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Houman Rezaizadeh indicated no relevant financial relationships.
Ruchir Damjibhai. Paladiya, MBBS1, Houman Rezaizadeh, MD2. P4027 - Acute Eosinophilic Appendicitis (AEA) Unmasking Eosinophilic Gastrointestinal Disorder (EGID) in a Misdiagnosed Case!, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
