Tuesday Poster Session
Category: Esophagus
P4028 - Colonic Tubular Adenoma Causing Obstruction Within a Colonic Interposition
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AG
Alexander D. Grieme, DO
Baylor Scott & White Medical Center
Corpus Christi, TX
Presenting Author(s)
Alexander Grieme, DO1, Heather Cancienne, DO2, Eric Smith, MD3, Henry Hinkle, MD4
1Baylor Scott & White Medical Center, Corpus Christi, TX; 2University Medical Center, New Orleans, LA; 3Baylor Scott & White Medical Center, Round Rock, TX; 4Saint Francis Health Systems, Monroe, LA
Introduction: Colonic interposition after esophagectomy is a relatively uncommon surgery. Pathologies such as esophageal atresia and esophageal stricture secondary to caustic ingestion necessitate reconstruction at young ages. Importantly, prolonged exposure to foreign materials increases the risk of adenocarcinoma in the colonic graft. This case highlights the importance of surveilling colonic grafts post-reconstruction as early detection and polypectomy reduce morbidity and mortality.
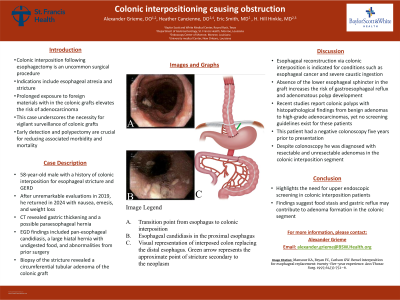
Case Description/Methods: The patient is a 58-year-old male with a past surgical history of colonic interposition secondary to esophageal stricture and GERD at 6 years old. In 2019 at age 53, routine EGD and colonoscopy were unremarkable. In 2024, the patient presented to the Emergency Department complaining of nausea and emesis. CT scan revealed nonspecific gastric thickening, possible paraesophageal hernia and esophageal diverticulum. At our clinic he endorsed epigastric fullness and regurgitation of undigested food particles after eating and weight loss. EGD revealed pan-esophageal candidiasis, a large hiatal hernia containing undigested food, evidence of previous colonic interposition surgery, a 5 mm polyp in the proximal colonic segment, and a circumferential polypoid mass at the distal aspect of the anastomosis. Pathology report confirmed tubular adenoma of the polyp and polypoid mass.
Discussion: Common indications for esophageal reconstruction via colonic interposition include esophageal cancer, esophageal atresia, end-stage stricturing disease and severe caustic ingestion. Absence of the lower esophageal sphincter in the colonic graft promotes reflux and likely increases the risk of adenomatous polyp formation. Recent publications report cases of colonic polyps in the interposed segment with histology ranging from benign adenomas to high-grade adenocarcinomas. Currently, no guidelines exist for screening or surveillance of a colonic interposition. Our patient presented with a history of negative screening colonoscopy 5 years prior to diagnosis of endoscopically resectable and unresectable adenomas within the interposed segment. Historically, fecal retention was thought to increase risk of polyp formation. In our patient it is reasonable to presume that food stasis and gastric reflux into the colonic graft may have contributed to adenoma formation. As evidenced by this case, adenomatous polyp formation occurs regardless of colon location, thus prompting the need for upper endoscopic screening in these patients.
Disclosures:
Alexander Grieme, DO1, Heather Cancienne, DO2, Eric Smith, MD3, Henry Hinkle, MD4. P4028 - Colonic Tubular Adenoma Causing Obstruction Within a Colonic Interposition, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor Scott & White Medical Center, Corpus Christi, TX; 2University Medical Center, New Orleans, LA; 3Baylor Scott & White Medical Center, Round Rock, TX; 4Saint Francis Health Systems, Monroe, LA
Introduction: Colonic interposition after esophagectomy is a relatively uncommon surgery. Pathologies such as esophageal atresia and esophageal stricture secondary to caustic ingestion necessitate reconstruction at young ages. Importantly, prolonged exposure to foreign materials increases the risk of adenocarcinoma in the colonic graft. This case highlights the importance of surveilling colonic grafts post-reconstruction as early detection and polypectomy reduce morbidity and mortality.
Case Description/Methods: The patient is a 58-year-old male with a past surgical history of colonic interposition secondary to esophageal stricture and GERD at 6 years old. In 2019 at age 53, routine EGD and colonoscopy were unremarkable. In 2024, the patient presented to the Emergency Department complaining of nausea and emesis. CT scan revealed nonspecific gastric thickening, possible paraesophageal hernia and esophageal diverticulum. At our clinic he endorsed epigastric fullness and regurgitation of undigested food particles after eating and weight loss. EGD revealed pan-esophageal candidiasis, a large hiatal hernia containing undigested food, evidence of previous colonic interposition surgery, a 5 mm polyp in the proximal colonic segment, and a circumferential polypoid mass at the distal aspect of the anastomosis. Pathology report confirmed tubular adenoma of the polyp and polypoid mass.
Discussion: Common indications for esophageal reconstruction via colonic interposition include esophageal cancer, esophageal atresia, end-stage stricturing disease and severe caustic ingestion. Absence of the lower esophageal sphincter in the colonic graft promotes reflux and likely increases the risk of adenomatous polyp formation. Recent publications report cases of colonic polyps in the interposed segment with histology ranging from benign adenomas to high-grade adenocarcinomas. Currently, no guidelines exist for screening or surveillance of a colonic interposition. Our patient presented with a history of negative screening colonoscopy 5 years prior to diagnosis of endoscopically resectable and unresectable adenomas within the interposed segment. Historically, fecal retention was thought to increase risk of polyp formation. In our patient it is reasonable to presume that food stasis and gastric reflux into the colonic graft may have contributed to adenoma formation. As evidenced by this case, adenomatous polyp formation occurs regardless of colon location, thus prompting the need for upper endoscopic screening in these patients.
Disclosures:
Alexander Grieme indicated no relevant financial relationships.
Heather Cancienne indicated no relevant financial relationships.
Eric Smith indicated no relevant financial relationships.
Henry Hinkle indicated no relevant financial relationships.
Alexander Grieme, DO1, Heather Cancienne, DO2, Eric Smith, MD3, Henry Hinkle, MD4. P4028 - Colonic Tubular Adenoma Causing Obstruction Within a Colonic Interposition, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
