Tuesday Poster Session
Category: Esophagus
P4029 - Acute Esophageal Necrosis: A Rare Case With an Unusual Challenge
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MM
Minni Meka, MD
Nova Southeastern University
Wellington, FL
Presenting Author(s)
Minni Meka, MD1, Sagar V. Mehta, MD2, Lissette Pola, DO1
1Nova Southeastern University, Wellington, FL; 2Wellington Regional Medical Center, Wellington, FL
Introduction: Acute esophageal necrosis (AEN), also known as Gurvits syndrome, is a rare clinical condition, with uncertain etiology. Rare in itself, this case report also highlights navigation of a unique clinical situation requiring trans-esophageal echocardiography (TEE) for Methicillin resistant Staphylococcus Aureus (MRSA) bacteremia.
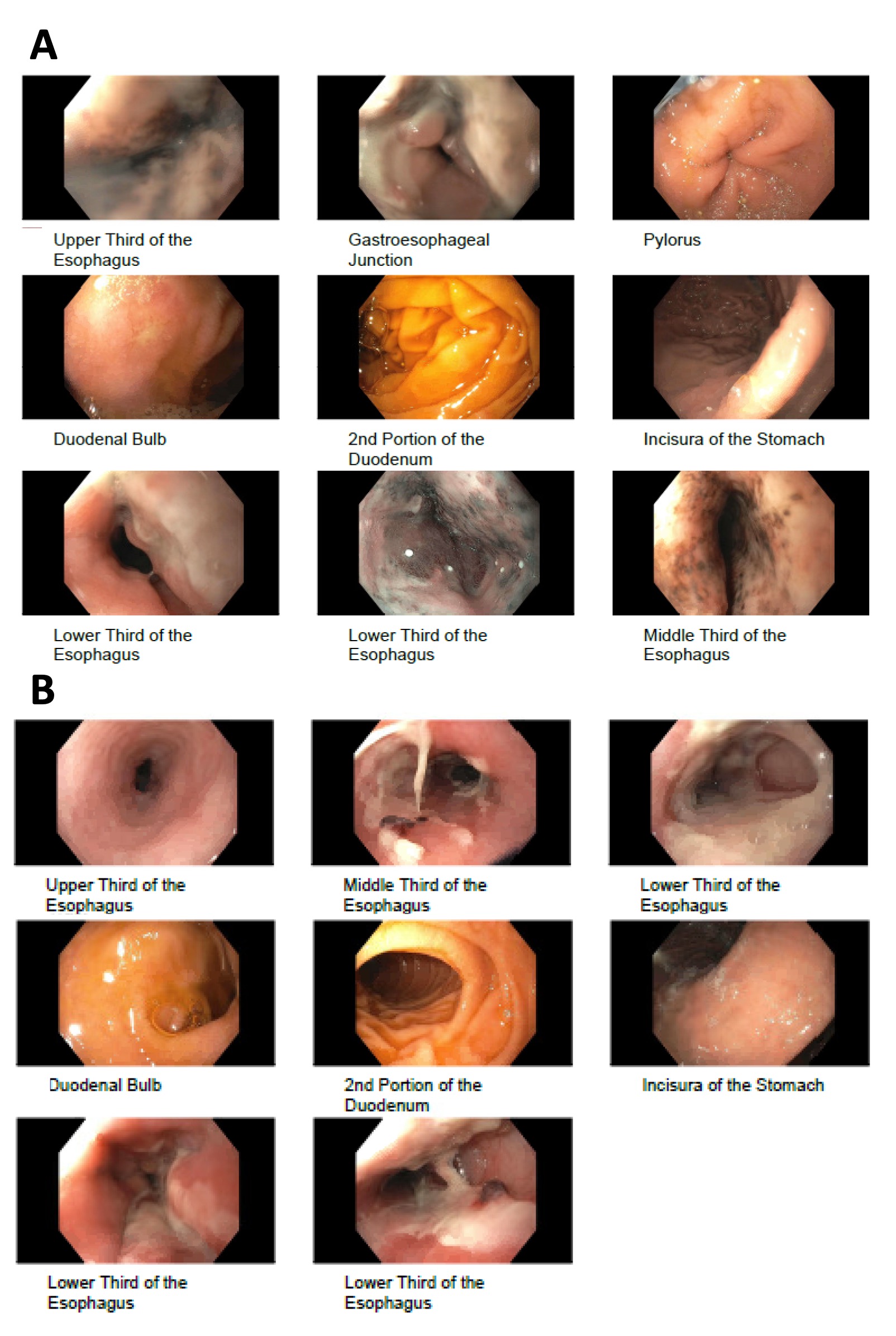
Case Description/Methods: Patient is a 69-year-old male presenting with 1 day history of upper abdominal pain, nausea, coffee-ground emesis. Prior medical history includes Type 2 diabetes mellitus, coronary artery disease, status post permanent pace maker insertion, chronic low back pain. Patient reported taking NSAIDs, Percocet and aspirin. On admission we noted a hemoglobin of 9.5 g/dl, a drop from previous hemoglobin of 11.6 g/dl 1 month ago, as well as an increase in Blood urea nitrogen (BUN) from 27 to 56. Esophagogastroduodenoscopy (EGD) revealed severe esophagitis, blackened necrotic appearing mucosa. Histology was consistent with tissue necrosis. A diagnosis of AEN was made. The patient received nothing by mouth and an intravenous (IV) proton pump inhibitor (PPI). Patient’s clinical course took an interesting turn when blood cultures were positive for MRSA with an indication for TEE. Patient was deemed to be at high risk of esophageal complications and was transferred to a higher center for alternative cardiac imaging and pacemaker removal. Upon clinical improvement EGD performed 4 weeks later showed significant resolution of necrosis but with some residual esophagitis.
Discussion: AEN is a rare clinical entity arising in the setting of multiorgan dysfunction, ischemia, sepsis, diabetic ketoacidosis, trauma, toxic ingestion and/or volume depletion that leads to ischemia and necrosis. Notable symptoms are upper gastrointestinal bleeding, melena, nausea, vomiting, dysphagia, abdominal pain. Diagnosis is made by EGD showing black circumferential esophagus in part or total extension to the gastroesophageal junction. Treatment includes systemic resuscitation with IV fluid therapy, glycemic control, use of IV PPI and parenteral nutrition. A mortality rate as high as 32% has been reported, likely related to comorbidities, acute complications such as perforation and mediastinitis. AEN should therefore be on the list of differential diagnoses for any upper GI bleeding. Also, in situations where a TEE is indicated as in this case, clinicians should be vigilant in avoiding the procedure and seeking alternative cardiac imaging modalities due to higher risk of complications.
Disclosures:
Minni Meka, MD1, Sagar V. Mehta, MD2, Lissette Pola, DO1. P4029 - Acute Esophageal Necrosis: A Rare Case With an Unusual Challenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nova Southeastern University, Wellington, FL; 2Wellington Regional Medical Center, Wellington, FL
Introduction: Acute esophageal necrosis (AEN), also known as Gurvits syndrome, is a rare clinical condition, with uncertain etiology. Rare in itself, this case report also highlights navigation of a unique clinical situation requiring trans-esophageal echocardiography (TEE) for Methicillin resistant Staphylococcus Aureus (MRSA) bacteremia.
Case Description/Methods: Patient is a 69-year-old male presenting with 1 day history of upper abdominal pain, nausea, coffee-ground emesis. Prior medical history includes Type 2 diabetes mellitus, coronary artery disease, status post permanent pace maker insertion, chronic low back pain. Patient reported taking NSAIDs, Percocet and aspirin. On admission we noted a hemoglobin of 9.5 g/dl, a drop from previous hemoglobin of 11.6 g/dl 1 month ago, as well as an increase in Blood urea nitrogen (BUN) from 27 to 56. Esophagogastroduodenoscopy (EGD) revealed severe esophagitis, blackened necrotic appearing mucosa. Histology was consistent with tissue necrosis. A diagnosis of AEN was made. The patient received nothing by mouth and an intravenous (IV) proton pump inhibitor (PPI). Patient’s clinical course took an interesting turn when blood cultures were positive for MRSA with an indication for TEE. Patient was deemed to be at high risk of esophageal complications and was transferred to a higher center for alternative cardiac imaging and pacemaker removal. Upon clinical improvement EGD performed 4 weeks later showed significant resolution of necrosis but with some residual esophagitis.
Discussion: AEN is a rare clinical entity arising in the setting of multiorgan dysfunction, ischemia, sepsis, diabetic ketoacidosis, trauma, toxic ingestion and/or volume depletion that leads to ischemia and necrosis. Notable symptoms are upper gastrointestinal bleeding, melena, nausea, vomiting, dysphagia, abdominal pain. Diagnosis is made by EGD showing black circumferential esophagus in part or total extension to the gastroesophageal junction. Treatment includes systemic resuscitation with IV fluid therapy, glycemic control, use of IV PPI and parenteral nutrition. A mortality rate as high as 32% has been reported, likely related to comorbidities, acute complications such as perforation and mediastinitis. AEN should therefore be on the list of differential diagnoses for any upper GI bleeding. Also, in situations where a TEE is indicated as in this case, clinicians should be vigilant in avoiding the procedure and seeking alternative cardiac imaging modalities due to higher risk of complications.
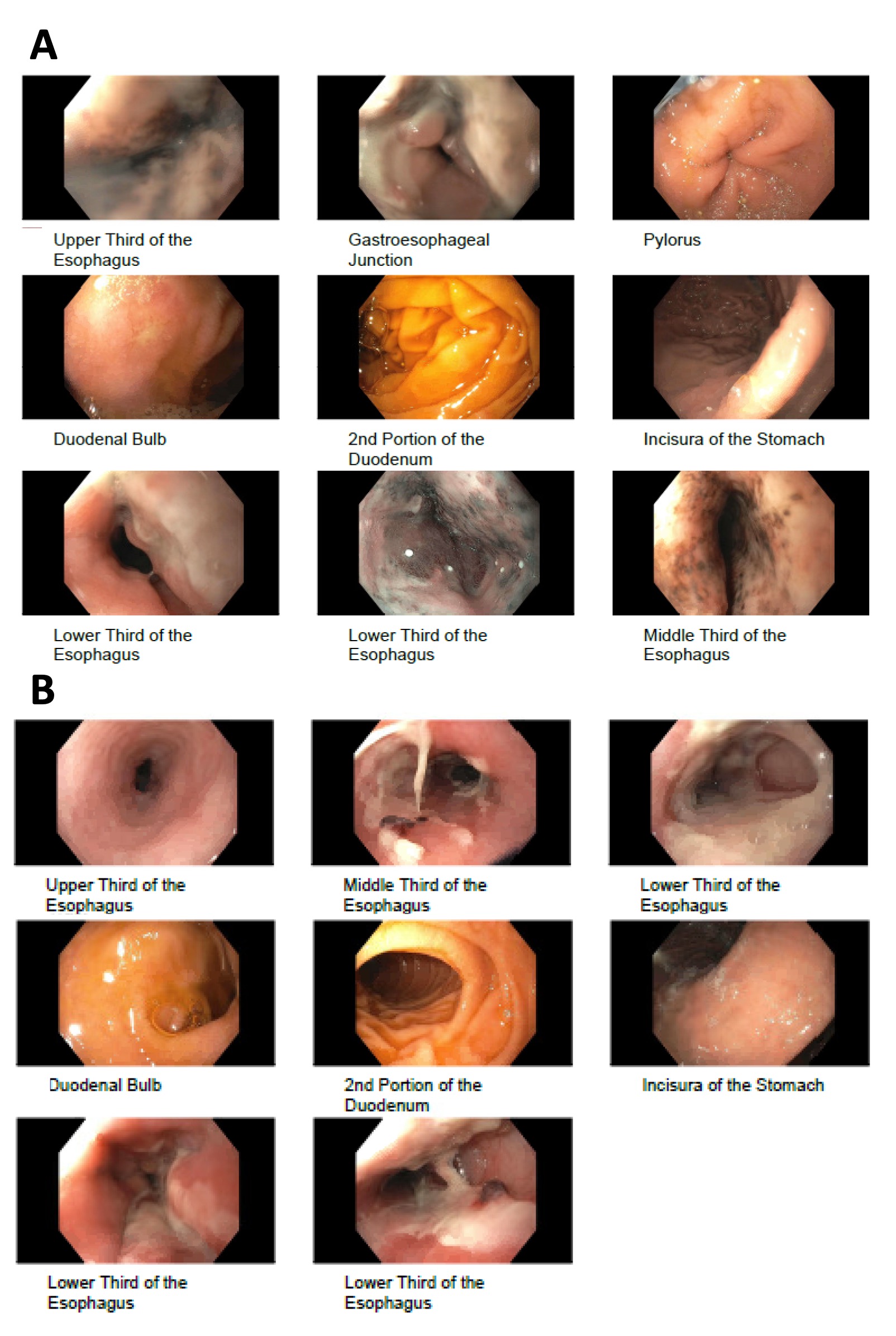
Figure: A-Initial EGD showing Severe esophagitis with no bleeding. This area was severely erosive and pigmented black.
B-Follow up EGD showing ulcerative esophagitis with friable mucosa throughout the mid and distal esophagus but no evidence of necrosis.
B-Follow up EGD showing ulcerative esophagitis with friable mucosa throughout the mid and distal esophagus but no evidence of necrosis.
Disclosures:
Minni Meka indicated no relevant financial relationships.
Sagar Mehta indicated no relevant financial relationships.
Lissette Pola indicated no relevant financial relationships.
Minni Meka, MD1, Sagar V. Mehta, MD2, Lissette Pola, DO1. P4029 - Acute Esophageal Necrosis: A Rare Case With an Unusual Challenge, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
