Tuesday Poster Session
Category: Esophagus
P4033 - Esophageal Intramural Pseudo-Diverticulosis Associated With Eosinophilic Esophagitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sandra Freeman, BA
Robert Wood Johnson Medical School, Rutgers University
New Brunwsick, NJ
Presenting Author(s)
Sandra Freeman, BA1, Anish V. Patel, MD2
1Robert Wood Johnson Medical School, Rutgers University, New Brunwsick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Esophageal Intramural Pseudo-diverticulosis (EIP) is a disease characterized by multiple small outpouchings of the esophagus with dilated execratory ducts of the submucosal gland. It is typically associated with underlying pathology. Few cases have been reported of eosinophilic esophagitis (EoE) occurring concomitantly with EIP.
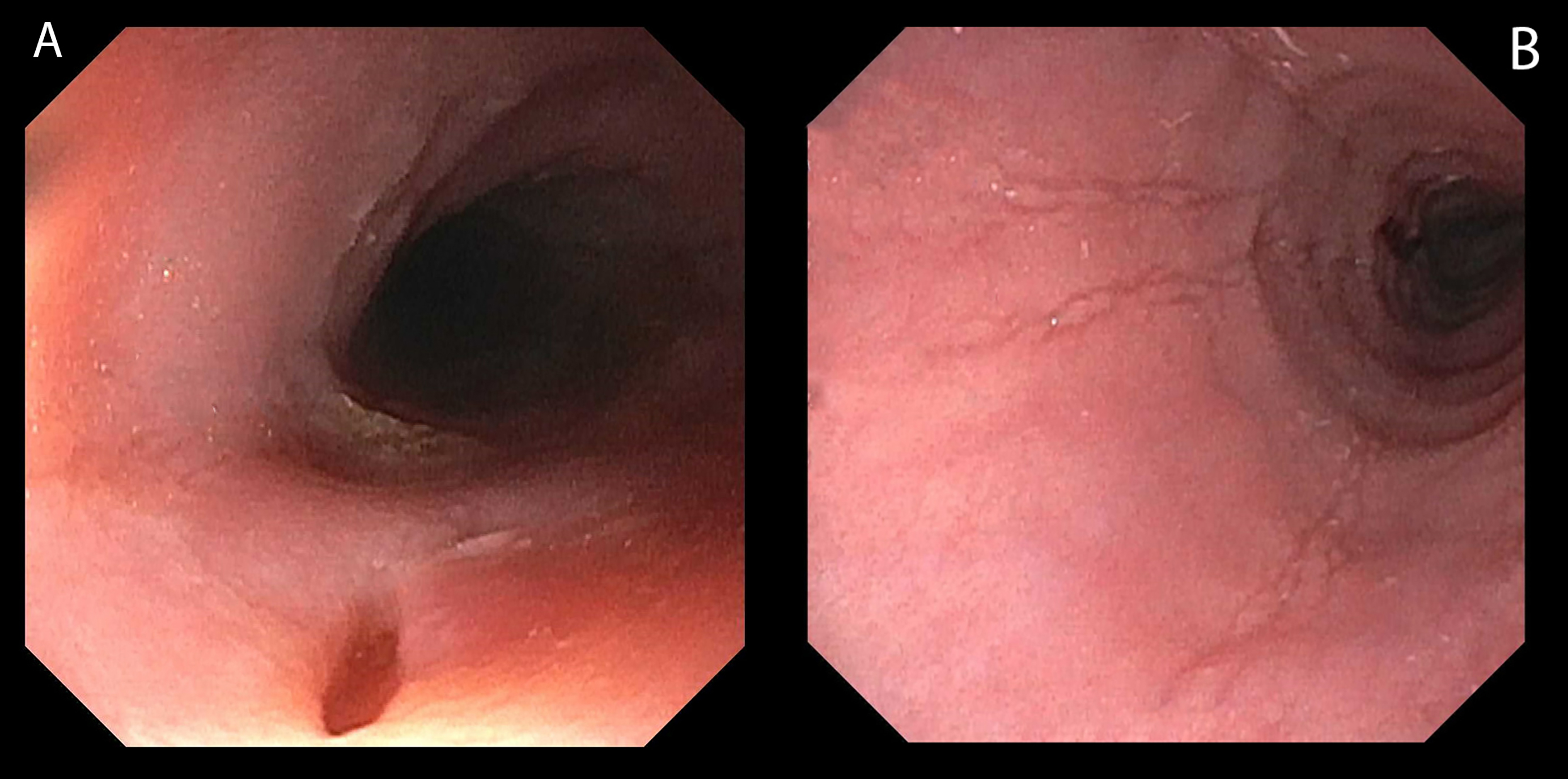
Case Description/Methods: A 25-year-old male with a history of seasonal allergies and allergic rhinitis was admitted for acute dysphagia and suspected esophageal food bolus impaction. After a meal, he felt like food was stuck in his esophagus and was subsequently unable to swallow liquids. He had two prior episodes that self-resolved. When admitted, he was taking cetirizine and albuterol, had no prior surgeries, and no history of smoking or alcohol use. He denied abdominal pain, hematemesis, melena, and hematochezia. He appeared in mild distress, but the rest of the physical exam was normal. Laboratories were remarkable for eosinophilia (9.9%). Esophagogastroduodenoscopy (EGD) was performed and strikingly showed multiple diverticula in the proximal and mid-esophagus (Figure 1A), along with longitudinal furrows and ringed mucosa throughout the esophagus (Figure 1B). Biopsies showed proximal, mid and distal esophageal mucosa with 40, 35 and 50 eosinophils/hpf, respectively, and was negative for cytomegalovirus (CMV), herpes simplex virus (HSV), and candidiasis. The patient was started on omeprazole 40mg twice daily and a follow-up EGD was scheduled in three for surveillance.
Discussion: We present here a rare association of EIP with underlying EoE. EIP is associated with pathology including infectious esophagitis, esophageal strictures and dysmotility. EIP is noted as visible outpouchings during endoscopy, but can be missed due to small size of the orifices. A thorough endoscopic evaluation of the esophagus is essential. Endoscopists must be aware of this disease entity, and obtain esophageal biopsies to rule out conditions including EoE as with our patient. If esophageal biopsies are normal, further investigation with XR esophagram and esophageal manometry should be considered. When evaluating a patient with dysphagia, a comprehensive workup is important for determining the underlying pathology, and it is important to identify uncommon conditions such as EIP. Furthermore, when EIP is diagnosed, periodic surveillance EGD should be considered given its association with esophageal carcinoma.
Disclosures:
Sandra Freeman, BA1, Anish V. Patel, MD2. P4033 - Esophageal Intramural Pseudo-Diverticulosis Associated With Eosinophilic Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Robert Wood Johnson Medical School, Rutgers University, New Brunwsick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Esophageal Intramural Pseudo-diverticulosis (EIP) is a disease characterized by multiple small outpouchings of the esophagus with dilated execratory ducts of the submucosal gland. It is typically associated with underlying pathology. Few cases have been reported of eosinophilic esophagitis (EoE) occurring concomitantly with EIP.
Case Description/Methods: A 25-year-old male with a history of seasonal allergies and allergic rhinitis was admitted for acute dysphagia and suspected esophageal food bolus impaction. After a meal, he felt like food was stuck in his esophagus and was subsequently unable to swallow liquids. He had two prior episodes that self-resolved. When admitted, he was taking cetirizine and albuterol, had no prior surgeries, and no history of smoking or alcohol use. He denied abdominal pain, hematemesis, melena, and hematochezia. He appeared in mild distress, but the rest of the physical exam was normal. Laboratories were remarkable for eosinophilia (9.9%). Esophagogastroduodenoscopy (EGD) was performed and strikingly showed multiple diverticula in the proximal and mid-esophagus (Figure 1A), along with longitudinal furrows and ringed mucosa throughout the esophagus (Figure 1B). Biopsies showed proximal, mid and distal esophageal mucosa with 40, 35 and 50 eosinophils/hpf, respectively, and was negative for cytomegalovirus (CMV), herpes simplex virus (HSV), and candidiasis. The patient was started on omeprazole 40mg twice daily and a follow-up EGD was scheduled in three for surveillance.
Discussion: We present here a rare association of EIP with underlying EoE. EIP is associated with pathology including infectious esophagitis, esophageal strictures and dysmotility. EIP is noted as visible outpouchings during endoscopy, but can be missed due to small size of the orifices. A thorough endoscopic evaluation of the esophagus is essential. Endoscopists must be aware of this disease entity, and obtain esophageal biopsies to rule out conditions including EoE as with our patient. If esophageal biopsies are normal, further investigation with XR esophagram and esophageal manometry should be considered. When evaluating a patient with dysphagia, a comprehensive workup is important for determining the underlying pathology, and it is important to identify uncommon conditions such as EIP. Furthermore, when EIP is diagnosed, periodic surveillance EGD should be considered given its association with esophageal carcinoma.
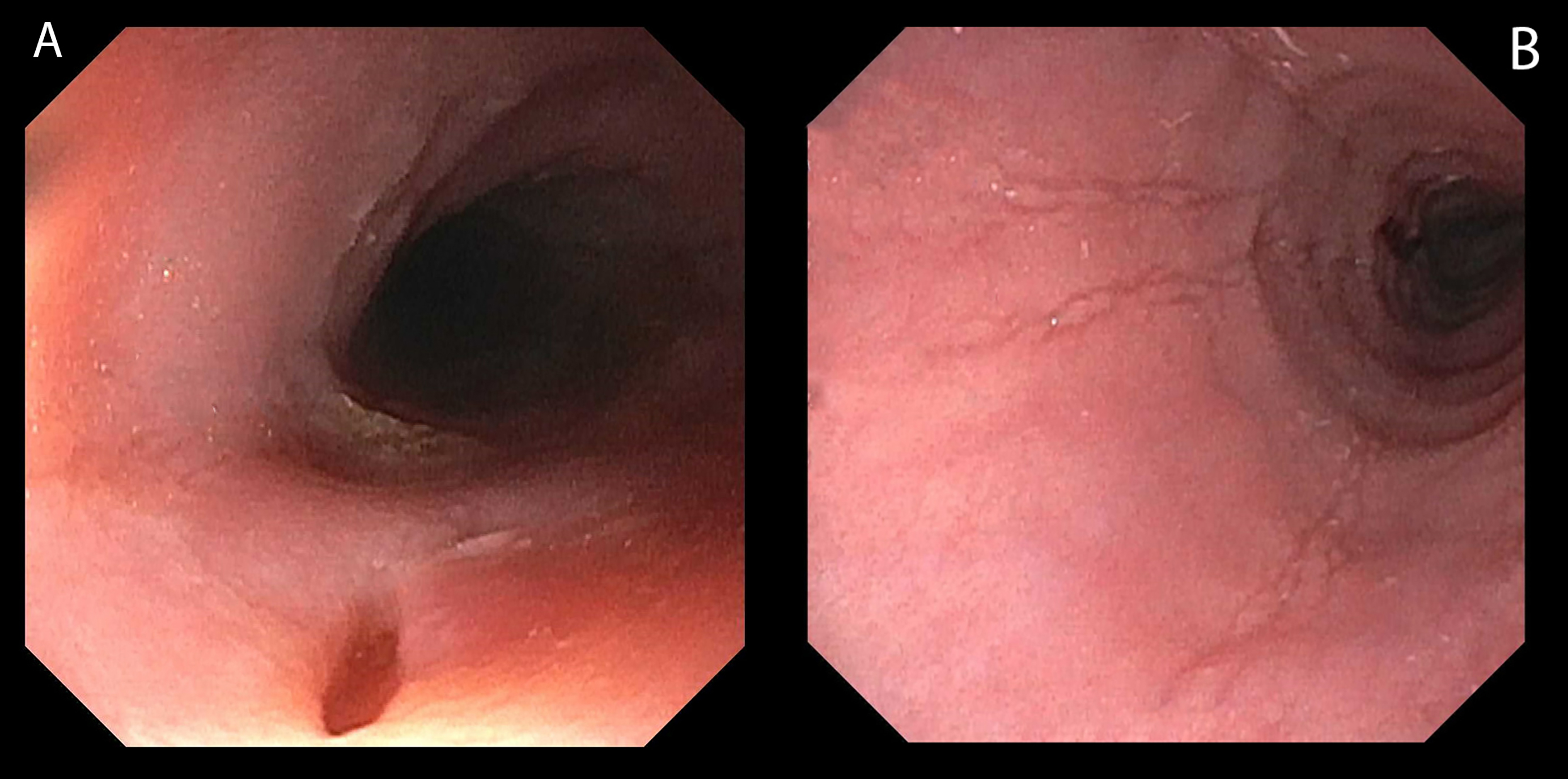
Figure: Figure 1: [A] Diverticula noted in the proximal and mid esophagus - representative diverticulum depicted here. [B] Longitudinal furrows noted in the mucosa throughout the esophagus. This was biopsied.
Disclosures:
Sandra Freeman indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Sandra Freeman, BA1, Anish V. Patel, MD2. P4033 - Esophageal Intramural Pseudo-Diverticulosis Associated With Eosinophilic Esophagitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
