Tuesday Poster Session
Category: Esophagus
P4037 - Esophageal Stenting for Acute Refractory Esophageal Variceal Bleeding: Opening a Bridge to Definitive Therapy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Oana Vester, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Oana Vester, MD, Vivek Mendiratta, MD, Chathur Acharya, MBBS
The Ohio State University Wexner Medical Center, Columbus, OH
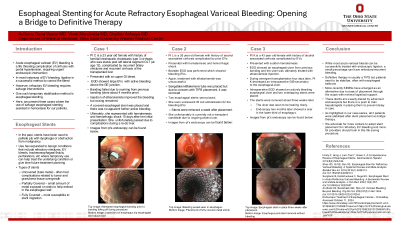
Introduction: Esophageal variceal (EV) bleeding is a life threating sequela of decompensated cirrhosis. Urgent EGD and band ligation is the recommended therapy. Refractory EV bleeding requires salvage interventions such as TIPS. Traditionally, placement of esophageal balloons has been the bridge therapy, but there are logistical issues and lack of expertise. Recently, through the scope esophageal stenting with self-expanding metal stents (SEMS) have become a viable option. We present 3 cases where the use of SEMS assisted in hemostasis.
Case Description/Methods: A 23 year old female with history of familial intrahepatic cholestasis cirrhosis who was s/p OLT (at age 12), c/b recurrent biliary stricture and cirrhosis of the transplanted liver, presented with an upper GI bleed. Emergent EGD found bleeding EVs. Banding failed and oozing remained after injection of ethanolamide. SEMS was pursed and there was no further bleeding after placement. She discharged but represented with hematemesis due to stent migration.
A 26 year old female with history of alcohol associated cirrhosis presented with hematemesis and hemorrhagic shock. Bedside EGD showed bleeding EVs. Treatment with ethalonlamine was unsuccessful. Sengstaken-Blakemore tube was placed but was removed due to concern with TIPS placement. 2 SEMS were placed. She underwent IR coil embolization for the EVs and SEMS were removed a week later.
A 43 year old female with history of alcohol associated cirrhosis presented with sudden hematemesis. EGD showed an esophageal ulcer from previous banding. Injection of epinephrine led to an actively bleeding vessel, so the ulcer was treated with ethanolamine injection. During emergent transplantation 4 days later, the patient developed an intraoperative GIB and EGD showed a bleeding esophageal ulcer. 2 overlapping SEMS were placed. The stents were removed weeks later and the ulcer was healing.
Discussion: While most variceal bleeds are successfully treated with endoscopic ligation, a small percentage have refractory bleeding. Definitive therapy is TIPS but patients need to be stabilized with esophageal balloons. Recently SEMSs have emerged as an alternative due to ease of placement through the scope with minimal logistical support. There is a push to train hepatologists in placing them to prevent delay in care. As highlighted in our case series, all 3 patients stabilized after stent placement. We advocate for more centers to adopt stent placement for refractory EV bleeding and train more providers in this procedure.
Disclosures:
Oana Vester, MD, Vivek Mendiratta, MD, Chathur Acharya, MBBS. P4037 - Esophageal Stenting for Acute Refractory Esophageal Variceal Bleeding: Opening a Bridge to Definitive Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Esophageal variceal (EV) bleeding is a life threating sequela of decompensated cirrhosis. Urgent EGD and band ligation is the recommended therapy. Refractory EV bleeding requires salvage interventions such as TIPS. Traditionally, placement of esophageal balloons has been the bridge therapy, but there are logistical issues and lack of expertise. Recently, through the scope esophageal stenting with self-expanding metal stents (SEMS) have become a viable option. We present 3 cases where the use of SEMS assisted in hemostasis.
Case Description/Methods: A 23 year old female with history of familial intrahepatic cholestasis cirrhosis who was s/p OLT (at age 12), c/b recurrent biliary stricture and cirrhosis of the transplanted liver, presented with an upper GI bleed. Emergent EGD found bleeding EVs. Banding failed and oozing remained after injection of ethanolamide. SEMS was pursed and there was no further bleeding after placement. She discharged but represented with hematemesis due to stent migration.
A 26 year old female with history of alcohol associated cirrhosis presented with hematemesis and hemorrhagic shock. Bedside EGD showed bleeding EVs. Treatment with ethalonlamine was unsuccessful. Sengstaken-Blakemore tube was placed but was removed due to concern with TIPS placement. 2 SEMS were placed. She underwent IR coil embolization for the EVs and SEMS were removed a week later.
A 43 year old female with history of alcohol associated cirrhosis presented with sudden hematemesis. EGD showed an esophageal ulcer from previous banding. Injection of epinephrine led to an actively bleeding vessel, so the ulcer was treated with ethanolamine injection. During emergent transplantation 4 days later, the patient developed an intraoperative GIB and EGD showed a bleeding esophageal ulcer. 2 overlapping SEMS were placed. The stents were removed weeks later and the ulcer was healing.
Discussion: While most variceal bleeds are successfully treated with endoscopic ligation, a small percentage have refractory bleeding. Definitive therapy is TIPS but patients need to be stabilized with esophageal balloons. Recently SEMSs have emerged as an alternative due to ease of placement through the scope with minimal logistical support. There is a push to train hepatologists in placing them to prevent delay in care. As highlighted in our case series, all 3 patients stabilized after stent placement. We advocate for more centers to adopt stent placement for refractory EV bleeding and train more providers in this procedure.
Disclosures:
Oana Vester indicated no relevant financial relationships.
Vivek Mendiratta indicated no relevant financial relationships.
Chathur Acharya indicated no relevant financial relationships.
Oana Vester, MD, Vivek Mendiratta, MD, Chathur Acharya, MBBS. P4037 - Esophageal Stenting for Acute Refractory Esophageal Variceal Bleeding: Opening a Bridge to Definitive Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
