Tuesday Poster Session
Category: Esophagus
P4038 - Circumferential Esophageal Gastric Inlet Patch Resulting in Upper Esophageal Stricture
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- GM
Giri Movva, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Giri Movva, MD1, Shiv Patel, BSA2, Keegan Colletier, MD1, Suimin Qiu, MD, PhD1, Sreeram Parupudi, MD1
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX
Introduction: Gastric inlet patch is a rare disorder that is seen between < 0.1% to 10% of adults. It is usually found in the proximal esophagus but can be found in other parts of the gastrointestinal tract. Typically, these patches appear localized and non-circumferential and can be incidental findings. However, the inlet patch can secrete acid leading to complications such as strictures, ulceration, perforation, and malignancy. Here, we present a rare case of esophageal stenosis caused by a circumferential gastric inlet patch.
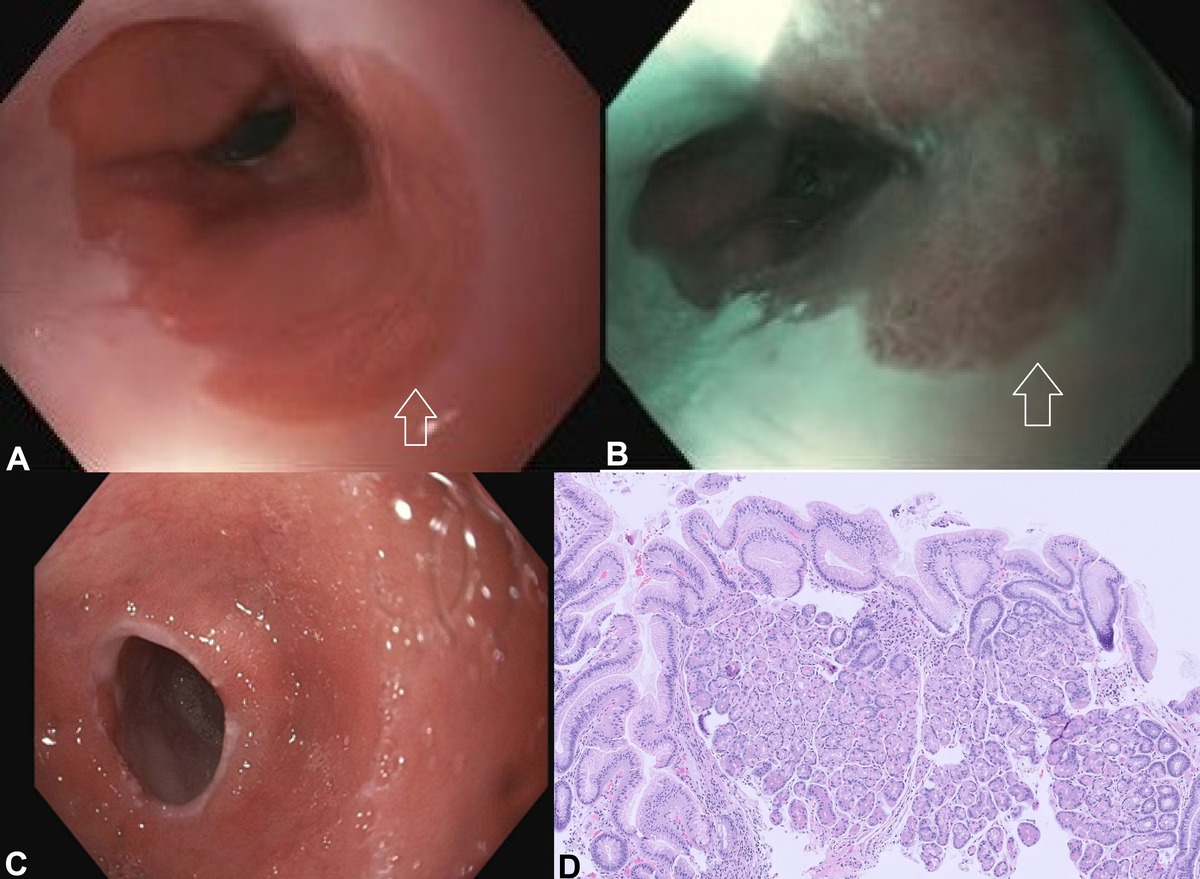
Case Description/Methods: A 69-year-old woman with a 30-year history of gastroesophageal reflux disease presented to the gastrointestinal clinic for worsening dysphagia to solids and pills. She was not taking any anti-reflux medications. She denied weight loss, nausea, vomiting, abdominal pain, melena, and hematochezia. Physical exam and labs were unremarkable. She underwent an esophagogastroduodenoscopy (EGD) which showed an irregular, circumferential area of ectopic gastric mucosa in the upper third of the esophagus 15-17 cm from the incisors and severe stenosis at 17 cm from incisors measuring 8mm in diameter and < 1cm in length (Figure 1A-C). A through-the-scope balloon dilator was passed through the stenosis with dilation up to 12mm with moderate improvement in the luminal narrowing. The patient was prescribed a proton pump inhibitor. Repeat EGD 1 month later demonstrated stenosis at 17 cm from incisors and was dilated again up to 15mm. The patient followed up in clinic and reported near resolution of symptoms. The biopsy of the stricture and proximal salmon-colored mucosa showed gastric-type mucosa with foveolar mucinous cells and parietal and chief cells (Figure 1D).
Discussion: Gastric inlet patches are relatively small and usually appear as isolated non-circumferential patches of salmon-colored mucosa. Most are found incidentally, but those thought to contribute to reflux symptoms can be treated with antacid therapy. In rare instances, larger circumferential gastric inlet patches can occur, and resultant strictures associated with dysphagia can develop, requiring dilation for symptomatic improvement. If symptoms are refractory, endoscopic mucosal resection and radiofrequency ablation can be considered. This case highlights an unusual circumferential gastric inlet patch causing esophageal stenosis and dysphagia. In a patient with chronic reflux symptoms, it shows the importance of considering this rare diagnosis and for early recognition to reduce the risk of complications.
Disclosures:
Giri Movva, MD1, Shiv Patel, BSA2, Keegan Colletier, MD1, Suimin Qiu, MD, PhD1, Sreeram Parupudi, MD1. P4038 - Circumferential Esophageal Gastric Inlet Patch Resulting in Upper Esophageal Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, John Sealy School of Medicine, Galveston, TX
Introduction: Gastric inlet patch is a rare disorder that is seen between < 0.1% to 10% of adults. It is usually found in the proximal esophagus but can be found in other parts of the gastrointestinal tract. Typically, these patches appear localized and non-circumferential and can be incidental findings. However, the inlet patch can secrete acid leading to complications such as strictures, ulceration, perforation, and malignancy. Here, we present a rare case of esophageal stenosis caused by a circumferential gastric inlet patch.
Case Description/Methods: A 69-year-old woman with a 30-year history of gastroesophageal reflux disease presented to the gastrointestinal clinic for worsening dysphagia to solids and pills. She was not taking any anti-reflux medications. She denied weight loss, nausea, vomiting, abdominal pain, melena, and hematochezia. Physical exam and labs were unremarkable. She underwent an esophagogastroduodenoscopy (EGD) which showed an irregular, circumferential area of ectopic gastric mucosa in the upper third of the esophagus 15-17 cm from the incisors and severe stenosis at 17 cm from incisors measuring 8mm in diameter and < 1cm in length (Figure 1A-C). A through-the-scope balloon dilator was passed through the stenosis with dilation up to 12mm with moderate improvement in the luminal narrowing. The patient was prescribed a proton pump inhibitor. Repeat EGD 1 month later demonstrated stenosis at 17 cm from incisors and was dilated again up to 15mm. The patient followed up in clinic and reported near resolution of symptoms. The biopsy of the stricture and proximal salmon-colored mucosa showed gastric-type mucosa with foveolar mucinous cells and parietal and chief cells (Figure 1D).
Discussion: Gastric inlet patches are relatively small and usually appear as isolated non-circumferential patches of salmon-colored mucosa. Most are found incidentally, but those thought to contribute to reflux symptoms can be treated with antacid therapy. In rare instances, larger circumferential gastric inlet patches can occur, and resultant strictures associated with dysphagia can develop, requiring dilation for symptomatic improvement. If symptoms are refractory, endoscopic mucosal resection and radiofrequency ablation can be considered. This case highlights an unusual circumferential gastric inlet patch causing esophageal stenosis and dysphagia. In a patient with chronic reflux symptoms, it shows the importance of considering this rare diagnosis and for early recognition to reduce the risk of complications.
Figure: Figure 1: Gastric inlet patch (white arrow) and stenosis/stricture seen in EGD. A) White light imaging. B) Blue light imaging. C) Esophageal Stenosis/Stricture. D) Esophageal stricture and proximal salmon-colored mucosa biopsy showed gastric-type mucosa with surface foveolar mucinous cells and oxyntic-type glands with acid-producing parietal cells (pink) and chief cells (purple).
Disclosures:
Giri Movva indicated no relevant financial relationships.
Shiv Patel indicated no relevant financial relationships.
Keegan Colletier indicated no relevant financial relationships.
Suimin Qiu indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Giri Movva, MD1, Shiv Patel, BSA2, Keegan Colletier, MD1, Suimin Qiu, MD, PhD1, Sreeram Parupudi, MD1. P4038 - Circumferential Esophageal Gastric Inlet Patch Resulting in Upper Esophageal Stricture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
