Tuesday Poster Session
Category: Functional Bowel Disease
P4075 - A Case of Chronic Infection with Yersinia enterocolitica Misdiagnosed as Irritable Bowel Syndrome: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KD
Kathleen DiCaprio, DO, PhD
Albany Medical Center
Albany, NY
Presenting Author(s)
Kathleen DiCaprio, DO, PhD1, Ahmad Abulawi, MD1, Cynthia Carlyn, MD2, Christopher Ashley, MD3
1Albany Medical Center, Albany, NY; 2Albany Stratton VA Medical Center, Albany, NY; 3Albany Stratton Veterans Affairs Medical Center, Albany, NY
Introduction: Yersinia enterocolitica is a gram-negative rod, of family Enterobacteriaceae, that primarily causes gastrointestinal tract infections. A zoonotic agent, Y. enterocolitica can be transmitted from contaminated food and water, as well as a wide range of animals. Although a unique bacterial enteropathogen, it is a rare cause of self-limiting acute gastroenteritis and less commonly pseudoappendicitis. Here, we present a case of chronic infection with Y. enterocolitica misdiagnosed as irritable bowel syndrome (IBS).
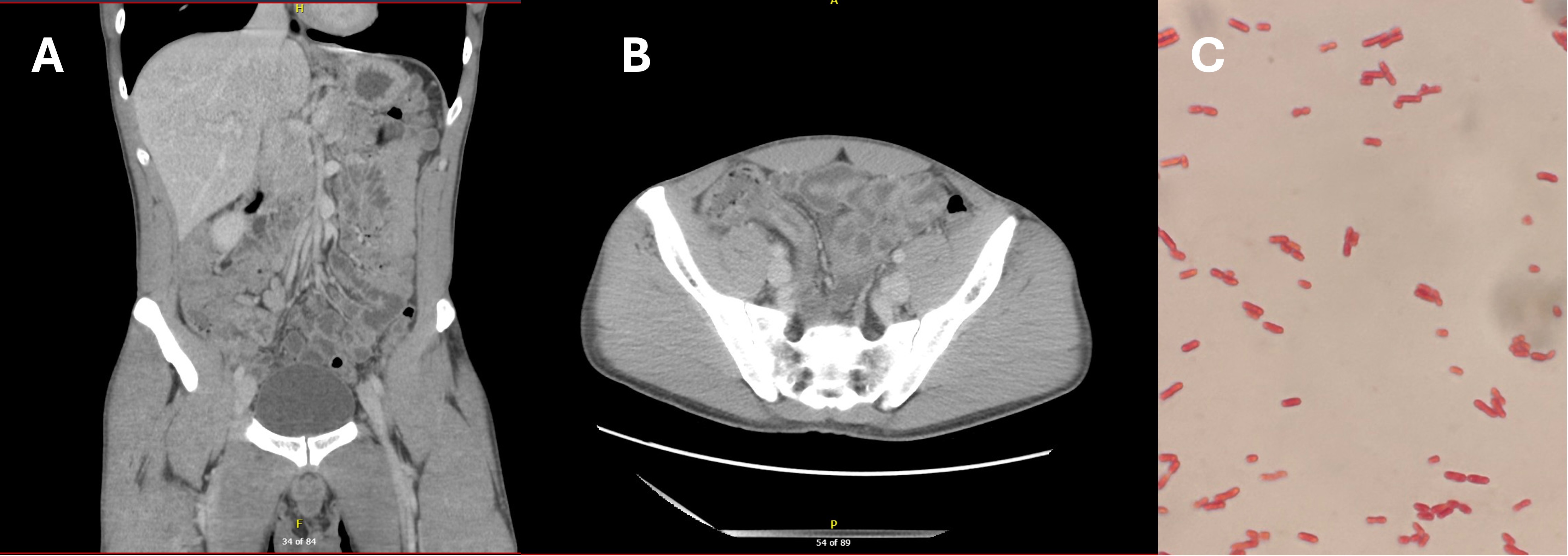
Case Description/Methods: A 28-year-old male with a history of chronic diarrhea, gastroesophageal reflux disease and IBS-D was admitted to the hospital with right lower quadrant abdominal pain and 1-day history of nausea and vomiting. The patient had a 3-year history of abdominal pain and diarrhea following most meals. Defecation often provided short term relief. He also had a 1-year history of 50lb weight loss due to voluntary restrictive eating to minimize daytime diarrhea. Prior evaluation with colonoscopy and endoscopy with biopsies were unrevealing, and he had been diagnosed with IBS-D. At admission, laboratory investigation revealed leukocytosis with neutrophil predominance, elevated C-reactive protein, positive calprotectin and negative for occult blood. The patient was alert, oriented and afebrile with moderate pain in the right lower quadrant without guarding or rebound tenderness during physical examination. Computed tomography abdomen/pelvis findings demonstrated enterocolitis with ileitis and only minimal changes to appendix. A differential diagnosis that included early appendicitis, inflammatory bowel disease, or an autoimmune disease was established. Subsequent stool polymerase chain reaction testing using GI Bio Fire were positive for <em>Y. enterocolitica</em>. The patient started a 3-week treatment with ceftriaxone and, within 48hrs, demonstrated relief of abdominal pain and diarrhea. Indeed, the patient had solid stool in parallel to eating three meals a day for the first time since IBS-D diagnosis.
Discussion: This case highlights the potential of missing Y. enterocolitica as an underlying etiology for chronic diarrhea and the importance of evaluation with stool studies using the GI Bio Fire to increase the sensitivity in detecting possible microbial infectious etiologies. A distinctive aspect of this case is the possibility that the patient had chronic infection with Y. enterocolitica that went undiagnosed for years, in conjunction with a misleading diagnosis of IBS-D.
Disclosures:
Kathleen DiCaprio, DO, PhD1, Ahmad Abulawi, MD1, Cynthia Carlyn, MD2, Christopher Ashley, MD3. P4075 - A Case of Chronic Infection with <i>Yersinia enterocolitica</i> Misdiagnosed as Irritable Bowel Syndrome: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albany Medical Center, Albany, NY; 2Albany Stratton VA Medical Center, Albany, NY; 3Albany Stratton Veterans Affairs Medical Center, Albany, NY
Introduction: Yersinia enterocolitica is a gram-negative rod, of family Enterobacteriaceae, that primarily causes gastrointestinal tract infections. A zoonotic agent, Y. enterocolitica can be transmitted from contaminated food and water, as well as a wide range of animals. Although a unique bacterial enteropathogen, it is a rare cause of self-limiting acute gastroenteritis and less commonly pseudoappendicitis. Here, we present a case of chronic infection with Y. enterocolitica misdiagnosed as irritable bowel syndrome (IBS).
Case Description/Methods: A 28-year-old male with a history of chronic diarrhea, gastroesophageal reflux disease and IBS-D was admitted to the hospital with right lower quadrant abdominal pain and 1-day history of nausea and vomiting. The patient had a 3-year history of abdominal pain and diarrhea following most meals. Defecation often provided short term relief. He also had a 1-year history of 50lb weight loss due to voluntary restrictive eating to minimize daytime diarrhea. Prior evaluation with colonoscopy and endoscopy with biopsies were unrevealing, and he had been diagnosed with IBS-D. At admission, laboratory investigation revealed leukocytosis with neutrophil predominance, elevated C-reactive protein, positive calprotectin and negative for occult blood. The patient was alert, oriented and afebrile with moderate pain in the right lower quadrant without guarding or rebound tenderness during physical examination. Computed tomography abdomen/pelvis findings demonstrated enterocolitis with ileitis and only minimal changes to appendix. A differential diagnosis that included early appendicitis, inflammatory bowel disease, or an autoimmune disease was established. Subsequent stool polymerase chain reaction testing using GI Bio Fire were positive for <em>Y. enterocolitica</em>. The patient started a 3-week treatment with ceftriaxone and, within 48hrs, demonstrated relief of abdominal pain and diarrhea. Indeed, the patient had solid stool in parallel to eating three meals a day for the first time since IBS-D diagnosis.
Discussion: This case highlights the potential of missing Y. enterocolitica as an underlying etiology for chronic diarrhea and the importance of evaluation with stool studies using the GI Bio Fire to increase the sensitivity in detecting possible microbial infectious etiologies. A distinctive aspect of this case is the possibility that the patient had chronic infection with Y. enterocolitica that went undiagnosed for years, in conjunction with a misleading diagnosis of IBS-D.
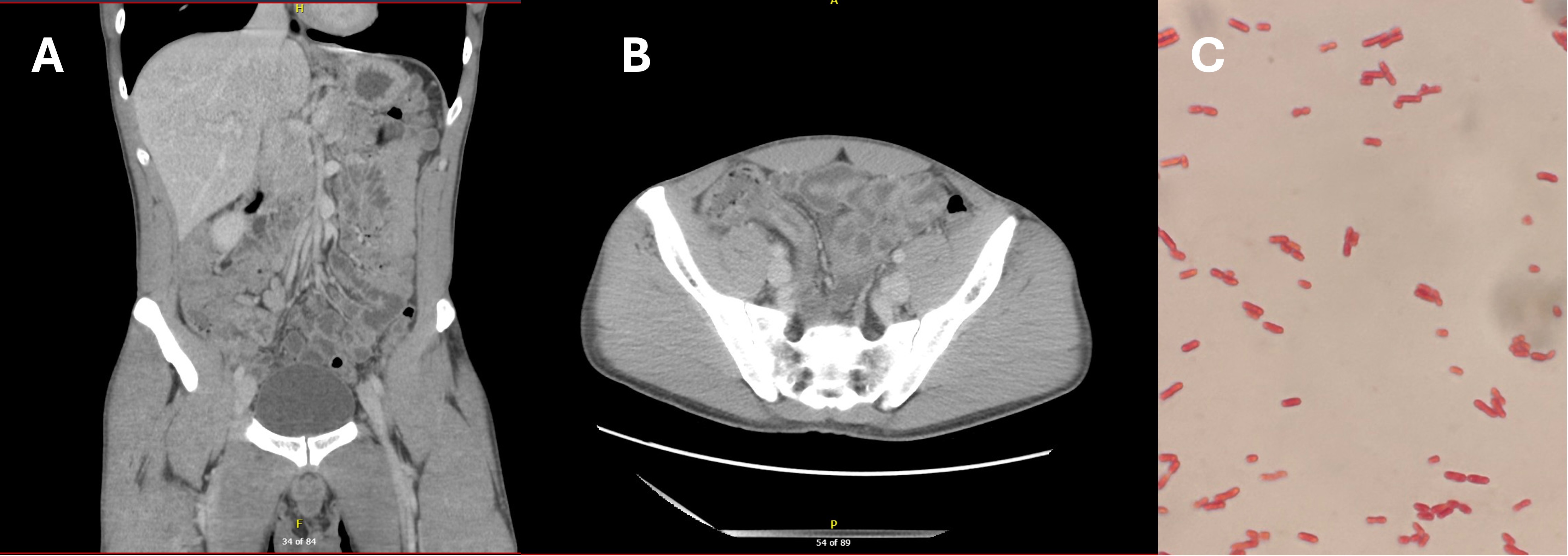
Figure: A) and B) Non-contrast CT Abdomen & Pelvis shows segmental wall thickening and hyperenhancement of ileum suggestive of ileitis as well as a thick-walled and decompressed ascending colon suggestive of enterocolitis. Small and large bowel with fluid contents. Mesenteric lymph nodes particularly at the ileocolic mesentery appear enlarged C) Gram-stained stool specimen reveals a field of numerous Gram-negative, rod shaped, Yersinia enterocolitica bacteria
Disclosures:
Kathleen DiCaprio indicated no relevant financial relationships.
Ahmad Abulawi indicated no relevant financial relationships.
Cynthia Carlyn indicated no relevant financial relationships.
Christopher Ashley indicated no relevant financial relationships.
Kathleen DiCaprio, DO, PhD1, Ahmad Abulawi, MD1, Cynthia Carlyn, MD2, Christopher Ashley, MD3. P4075 - A Case of Chronic Infection with <i>Yersinia enterocolitica</i> Misdiagnosed as Irritable Bowel Syndrome: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
