Tuesday Poster Session
Category: General Endoscopy
P4088 - Impact of a Standardized Inpatient Bowel Prep Order Set on Adequacy of Bowel Preparation for Colonoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Sarah Uttal, MD
Michigan Medicine
Ann Arbor, MI
Presenting Author(s)
Sarah Uttal, MD1, Jessica L. Sheehan, MD, MSc2, Fadi Hawa, MD2, Joyce J.. Kim, MD, MS3, Mehwish Ahmed, MD1, Tammy Ellies, 1, Shirley Cohen-Mekelburg, MD, MS1, Stacy Menees, MD1
1Michigan Medicine, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI; 3Michigan Medicine, Saline, MI
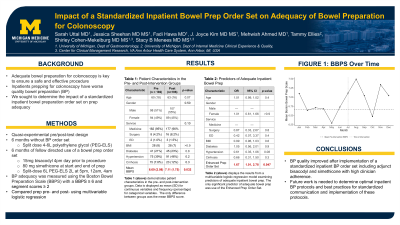
Introduction: Inpatients undergoing colonoscopy have worse bowel preparation quality than outpatients. However, an optimal bowel preparation regimen for inpatients has not been identified. We aimed to determine the impact of a standardized inpatient bowel preparation (BP) order set on BP adequacy.
Methods: We used a quasi-experimental pre/post-test design to examine the impact of a standardized inpatient BP order set using enhanced prep (split-dose 6 liters polyethylene glycol (PEG-ELS), 15mg bisacodyl, and 160 mg simethicone) on BP adequacy compared to PEG-ELS alone. Data on patient demographics, medication administration, order set usage, and BP adequacy were collected for 6 months pre- and post-intervention. BP adequacy was measured using the Boston Bowel Preparation Scale (BBPS) with a BBPS ≥ 6 and segment scores ≥ 2. We compared BP quality pre- and post-intervention using multivariable logistic regression and adjusting a priori for age, gender, race, admitting service, body mass index, and comorbidities.
Results: We included 388 inpatients undergoing colonoscopy, 192 (49.5%) pre-intervention and 196 (50.5%) post-intervention. A total of 183 (47%) of patients were female, 309 (80%) were white, and the mean age was 62 years (standard deviation 17). There were no differences in patient demographics between the pre- and post-intervention groups. The mean BBPS post intervention (7.11) was significantly greater than the mean BBPS pre-intervention (6.69) (t = -2.15, p = 0.03). When adjusting for patient factors (see Table), inpatients undergoing colonoscopy post-intervention were more likely to have an adequate BP compared to pre-intervention (odds ratio 1.66, confidence interval 1.00-2.79, p = 0.05). No other significant predictors of BP adequacy were identified. Finally, there was an overall high usage rate of the order set, with 85% of providers utilizing the standardized inpatient BP order set after its creation.
Discussion: We found that inpatient BP quality improved after implementation of a standardized inpatient BP order set including adjunct bisacodyl and simethicone with high clinician adherence. Future work is needed to determine optimal inpatient BP protocols and best practices for standardized communication and implementation of these protocols.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sarah Uttal, MD1, Jessica L. Sheehan, MD, MSc2, Fadi Hawa, MD2, Joyce J.. Kim, MD, MS3, Mehwish Ahmed, MD1, Tammy Ellies, 1, Shirley Cohen-Mekelburg, MD, MS1, Stacy Menees, MD1. P4088 - Impact of a Standardized Inpatient Bowel Prep Order Set on Adequacy of Bowel Preparation for Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Michigan Medicine, Ann Arbor, MI; 2University of Michigan, Ann Arbor, MI; 3Michigan Medicine, Saline, MI
Introduction: Inpatients undergoing colonoscopy have worse bowel preparation quality than outpatients. However, an optimal bowel preparation regimen for inpatients has not been identified. We aimed to determine the impact of a standardized inpatient bowel preparation (BP) order set on BP adequacy.
Methods: We used a quasi-experimental pre/post-test design to examine the impact of a standardized inpatient BP order set using enhanced prep (split-dose 6 liters polyethylene glycol (PEG-ELS), 15mg bisacodyl, and 160 mg simethicone) on BP adequacy compared to PEG-ELS alone. Data on patient demographics, medication administration, order set usage, and BP adequacy were collected for 6 months pre- and post-intervention. BP adequacy was measured using the Boston Bowel Preparation Scale (BBPS) with a BBPS ≥ 6 and segment scores ≥ 2. We compared BP quality pre- and post-intervention using multivariable logistic regression and adjusting a priori for age, gender, race, admitting service, body mass index, and comorbidities.
Results: We included 388 inpatients undergoing colonoscopy, 192 (49.5%) pre-intervention and 196 (50.5%) post-intervention. A total of 183 (47%) of patients were female, 309 (80%) were white, and the mean age was 62 years (standard deviation 17). There were no differences in patient demographics between the pre- and post-intervention groups. The mean BBPS post intervention (7.11) was significantly greater than the mean BBPS pre-intervention (6.69) (t = -2.15, p = 0.03). When adjusting for patient factors (see Table), inpatients undergoing colonoscopy post-intervention were more likely to have an adequate BP compared to pre-intervention (odds ratio 1.66, confidence interval 1.00-2.79, p = 0.05). No other significant predictors of BP adequacy were identified. Finally, there was an overall high usage rate of the order set, with 85% of providers utilizing the standardized inpatient BP order set after its creation.
Discussion: We found that inpatient BP quality improved after implementation of a standardized inpatient BP order set including adjunct bisacodyl and simethicone with high clinician adherence. Future work is needed to determine optimal inpatient BP protocols and best practices for standardized communication and implementation of these protocols.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sarah Uttal indicated no relevant financial relationships.
Jessica Sheehan indicated no relevant financial relationships.
Fadi Hawa indicated no relevant financial relationships.
Joyce Kim indicated no relevant financial relationships.
Mehwish Ahmed indicated no relevant financial relationships.
Tammy Ellies indicated no relevant financial relationships.
Shirley Cohen-Mekelburg indicated no relevant financial relationships.
Stacy Menees indicated no relevant financial relationships.
Sarah Uttal, MD1, Jessica L. Sheehan, MD, MSc2, Fadi Hawa, MD2, Joyce J.. Kim, MD, MS3, Mehwish Ahmed, MD1, Tammy Ellies, 1, Shirley Cohen-Mekelburg, MD, MS1, Stacy Menees, MD1. P4088 - Impact of a Standardized Inpatient Bowel Prep Order Set on Adequacy of Bowel Preparation for Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
