Tuesday Poster Session
Category: General Endoscopy
P4090 - The Impact of GLP-1 Receptor Agonists on Upper and Lower GI Endoscopy: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Bara A. Abujaber, MD
MedStar Health-Georgetown/Washington Hospital Center
Washington, DC
Presenting Author(s)
Spyridon Peppas, MD1, Bara Abujaber, MD1, Nadera Altork, MD1, Amer Arman, MD1, Sayel Alzraikat, MD1, Camille Boustani, MD2, Won Kyoo Cho, MD,3
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2MedStar Georgetown University Hospital, Washington, DC; 3Inova Health System/Georgetown University School of Medicine, Leesburg, VA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RA) are widely used oral anti-diabetic agents with increasing use for the management of obesity. Emerging literature suggests that GLP-1 RA may be associated with high gastric residue in the esophagogastroduodenoscopy (EGD) and potentially affect bowel preparation before a colonoscopy. Therefore, we aimed to investigate the influence of GLP-1 RA on the endoscopic procedures.
Methods: We performed a systematic review of the literature using Medline, Embase and Cochrane databases from inception to March 2024 to identify studies evaluating the effect of GLP-1 RA on EGD and bowel preparation for colonoscopy. We selected studies comparing gastric residue, satisfactory bowel preparation (Boston Bowel Preparation Scale, BBPS > 5) and mean BBPS scores between GLP-1 RA users versus non-users. Hedges’ g test was used to calculate the standardized mean difference of BBPS between the two groups. Random effects model was used and analysis was performed with STATA 17.
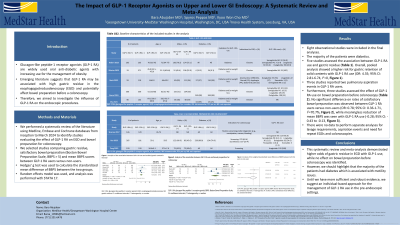
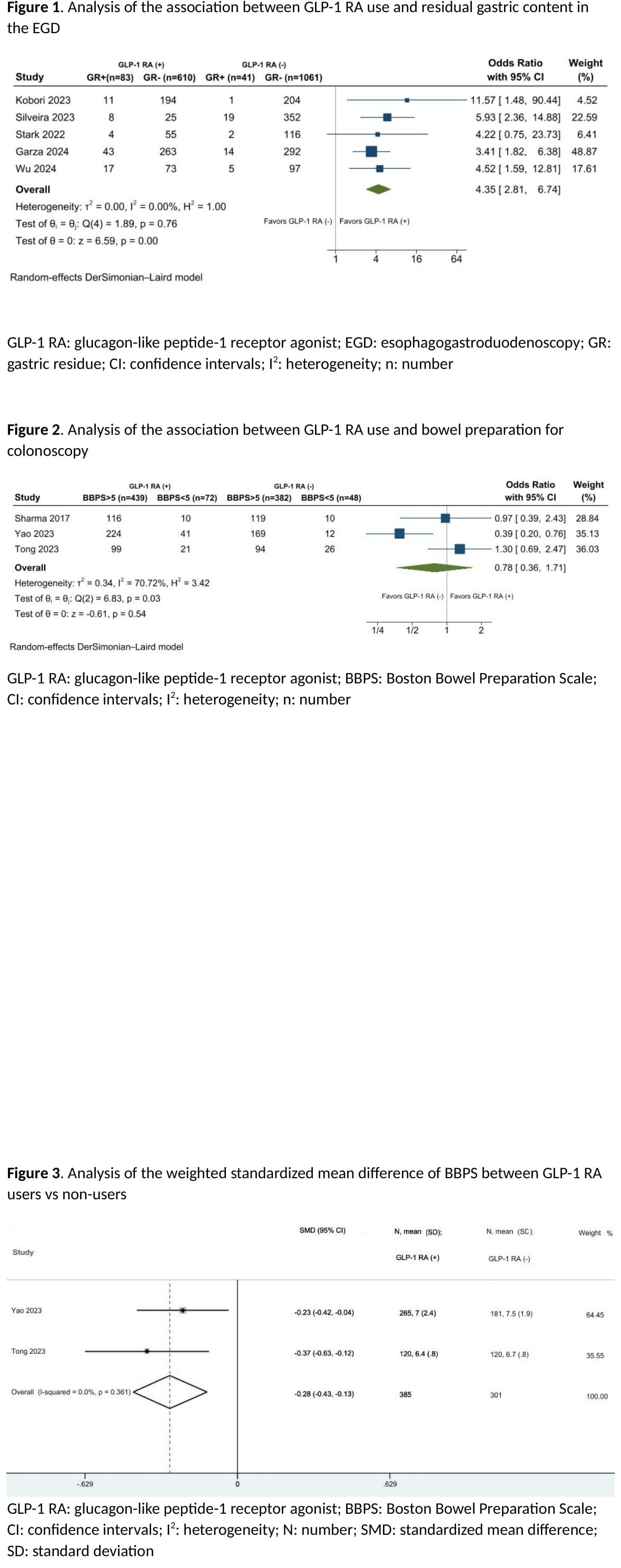
Results: Eight observational studies were included in the final analyses. The majority of the patients were diabetics. Five studies assessed the association between GLP-1 RA use and gastric residue. Overall, pooled analysis showed a higher risk for gastric retention of solid contents with GLP-1 RA use (OR: 4.35; 95% CI: 2.81-6.74, I2=0, Figure 1). Three studies reported two pulmonary aspiration events in GLP-1 RA users. Furthermore, three studies assessed the effect of GLP-1 RA use on bowel preparation before colonoscopy. No significant difference on rates of satisfactory bowel preparation was observed between GLP-1 RA users versus non-users (OR: 0.78; 95% CI: 0.36-1.71, I2=70.7%, Figure 2), while meaningless reduction of mean BBPS was seen with GLP-1 RA use (-0.28; 95% CI: -0.43 to -0.13, Figure 3). There were no data to perform separate analyses for lavage requirements, aspiration events and need for repeat EGDs and colonoscopies.
Discussion: This systematic review and meta-analysis demonstrated higher odds of gastric residue in EGD with GLP-1 use, while no effect on bowel preparation before colonoscopy was identified. However, we should highlight that the majority of the patients had diabetes which is associated with motility issues. Until we have more sufficient and robust evidence, we suggest an individual-based approach for the management of GLP-1 RA use in the pre-endoscopic settings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Spyridon Peppas, MD1, Bara Abujaber, MD1, Nadera Altork, MD1, Amer Arman, MD1, Sayel Alzraikat, MD1, Camille Boustani, MD2, Won Kyoo Cho, MD,3. P4090 - The Impact of GLP-1 Receptor Agonists on Upper and Lower GI Endoscopy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Health-Georgetown/Washington Hospital Center, Washington, DC; 2MedStar Georgetown University Hospital, Washington, DC; 3Inova Health System/Georgetown University School of Medicine, Leesburg, VA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RA) are widely used oral anti-diabetic agents with increasing use for the management of obesity. Emerging literature suggests that GLP-1 RA may be associated with high gastric residue in the esophagogastroduodenoscopy (EGD) and potentially affect bowel preparation before a colonoscopy. Therefore, we aimed to investigate the influence of GLP-1 RA on the endoscopic procedures.
Methods: We performed a systematic review of the literature using Medline, Embase and Cochrane databases from inception to March 2024 to identify studies evaluating the effect of GLP-1 RA on EGD and bowel preparation for colonoscopy. We selected studies comparing gastric residue, satisfactory bowel preparation (Boston Bowel Preparation Scale, BBPS > 5) and mean BBPS scores between GLP-1 RA users versus non-users. Hedges’ g test was used to calculate the standardized mean difference of BBPS between the two groups. Random effects model was used and analysis was performed with STATA 17.
Results: Eight observational studies were included in the final analyses. The majority of the patients were diabetics. Five studies assessed the association between GLP-1 RA use and gastric residue. Overall, pooled analysis showed a higher risk for gastric retention of solid contents with GLP-1 RA use (OR: 4.35; 95% CI: 2.81-6.74, I2=0, Figure 1). Three studies reported two pulmonary aspiration events in GLP-1 RA users. Furthermore, three studies assessed the effect of GLP-1 RA use on bowel preparation before colonoscopy. No significant difference on rates of satisfactory bowel preparation was observed between GLP-1 RA users versus non-users (OR: 0.78; 95% CI: 0.36-1.71, I2=70.7%, Figure 2), while meaningless reduction of mean BBPS was seen with GLP-1 RA use (-0.28; 95% CI: -0.43 to -0.13, Figure 3). There were no data to perform separate analyses for lavage requirements, aspiration events and need for repeat EGDs and colonoscopies.
Discussion: This systematic review and meta-analysis demonstrated higher odds of gastric residue in EGD with GLP-1 use, while no effect on bowel preparation before colonoscopy was identified. However, we should highlight that the majority of the patients had diabetes which is associated with motility issues. Until we have more sufficient and robust evidence, we suggest an individual-based approach for the management of GLP-1 RA use in the pre-endoscopic settings.
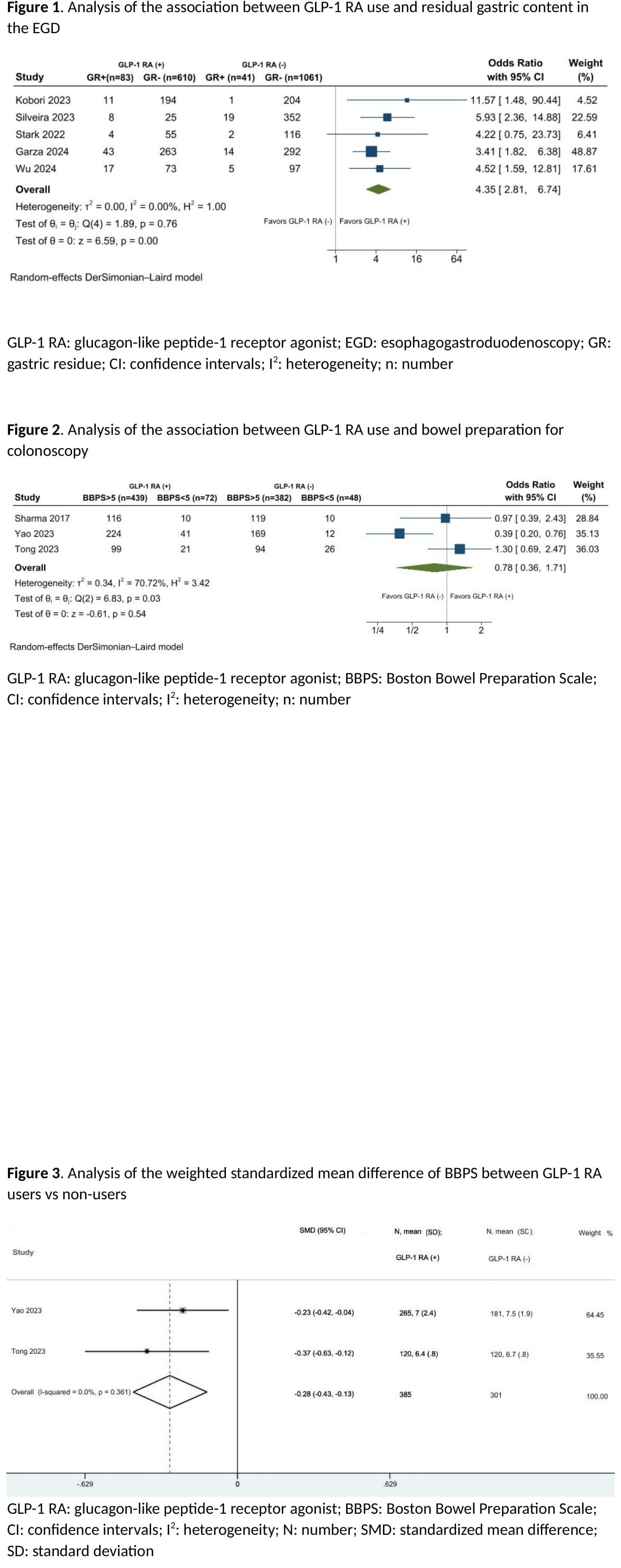
Figure: Figure 1. Analysis of the association between GLP-1 RA use and residual gastric content in the EGD
Figure 2. Analysis of the association between GLP-1 RA use and bowel preparation for colonoscopy
Figure 3. Analysis of the weighted standardized mean difference of BBPS between GLP-1 RA users vs non-users
Figure 2. Analysis of the association between GLP-1 RA use and bowel preparation for colonoscopy
Figure 3. Analysis of the weighted standardized mean difference of BBPS between GLP-1 RA users vs non-users
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Spyridon Peppas indicated no relevant financial relationships.
Bara Abujaber indicated no relevant financial relationships.
Nadera Altork indicated no relevant financial relationships.
Amer Arman indicated no relevant financial relationships.
Sayel Alzraikat indicated no relevant financial relationships.
Camille Boustani indicated no relevant financial relationships.
Won Kyoo Cho indicated no relevant financial relationships.
Spyridon Peppas, MD1, Bara Abujaber, MD1, Nadera Altork, MD1, Amer Arman, MD1, Sayel Alzraikat, MD1, Camille Boustani, MD2, Won Kyoo Cho, MD,3. P4090 - The Impact of GLP-1 Receptor Agonists on Upper and Lower GI Endoscopy: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
