Tuesday Poster Session
Category: General Endoscopy
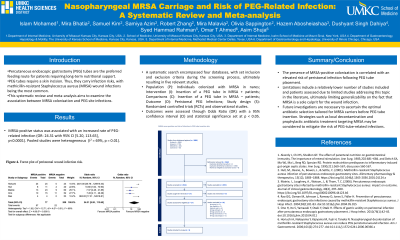
P4116 - Nasopharyngeal MRSA Carriage and Risk of PEG-Related Infection: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mira K. Bhatia, BA
University of Missouri - Kansas City School of Medicine
Presenting Author(s)
Islam Mohamed, MD1, Samuel J. Kim, BA2, Mira K. Bhatia, BA1, Samiya Azim, BA1, Robert Zhang, BA3, Mira Malavia, BA1, Olivia Sappington, BA1, Noor Hassan, MD3, Hazem Abosheaishaa, MD4, Dushyant S. Dahiya, MD5, Syed Hamaad Rahman, DO6, Omar T. Ahmed, MD7
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri-Kansas City School of Medicine, Kansas City, MO; 3University of Missouri Kansas City School of Medicine, Kansas City, MO; 4Icahn School of Medicine at Mount Sinai, Queens, NY; 5The University of Kansas School of Medicine, Kansas City, KS; 6Methodist Dallas Medical Center, Irving, TX; 7University of Illinois at Chicago, Chicago, IL
Introduction: Enteral feeding via percutaneous endoscopic gastrostomy (PEG) is preferred for patients requiring long-term nutritional support. However, PEG tube insertion carries infection risks, including methicillin-resistant Staphylococcus aureus (MRSA) wound infection. This systematic review and meta-analysis aims to examine the association between MRSA colonization and PEG site infections.
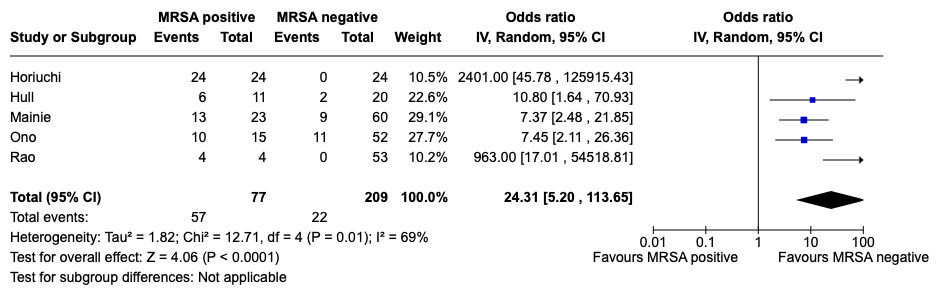
Methods: We conducted a systematic search across four major databases (Embase, Medline, Cochrane, and Scopus), focusing on MRSA colonization and PEG-related infections.Statistical analysis, employing RevMan v5.3, utilized mean differences for continuous outcomes and odds ratios for dichotomous outcomes, with random-effects models. Significance was set at p < 0.05. Heterogeneity was evaluated using I-square tests. Five studies comprising 286 patients were analyzed, with 77 tested positive for nasopharyngeal MRSA colonization and 209 tested negative.
Results: MRSA-positive status was significantly associated with a higher rate of PEG-related infection (OR: 24.31, 95% CI [5.20, 113.65], p < 0.0001). Our meta-analysis underscores the notable correlation between nasopharyngeal MRSA colonization and an increased risk of PEG-related infections.
Discussion: These findings emphasize the necessity of factoring in MRSA status when performing PEG insertion procedures. Healthcare providers should remain vigilant in implementing infection prevention strategies, especially in MRSA-positive patients, to reduce complications associated with PEG tube placements. Further investigation is needed to ascertain optimal preventive measures tailored to the MRSA colonization status within this patient cohort.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Islam Mohamed, MD1, Samuel J. Kim, BA2, Mira K. Bhatia, BA1, Samiya Azim, BA1, Robert Zhang, BA3, Mira Malavia, BA1, Olivia Sappington, BA1, Noor Hassan, MD3, Hazem Abosheaishaa, MD4, Dushyant S. Dahiya, MD5, Syed Hamaad Rahman, DO6, Omar T. Ahmed, MD7. P4116 - Nasopharyngeal MRSA Carriage and Risk of PEG-Related Infection: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri-Kansas City School of Medicine, Kansas City, MO; 3University of Missouri Kansas City School of Medicine, Kansas City, MO; 4Icahn School of Medicine at Mount Sinai, Queens, NY; 5The University of Kansas School of Medicine, Kansas City, KS; 6Methodist Dallas Medical Center, Irving, TX; 7University of Illinois at Chicago, Chicago, IL
Introduction: Enteral feeding via percutaneous endoscopic gastrostomy (PEG) is preferred for patients requiring long-term nutritional support. However, PEG tube insertion carries infection risks, including methicillin-resistant Staphylococcus aureus (MRSA) wound infection. This systematic review and meta-analysis aims to examine the association between MRSA colonization and PEG site infections.
Methods: We conducted a systematic search across four major databases (Embase, Medline, Cochrane, and Scopus), focusing on MRSA colonization and PEG-related infections.Statistical analysis, employing RevMan v5.3, utilized mean differences for continuous outcomes and odds ratios for dichotomous outcomes, with random-effects models. Significance was set at p < 0.05. Heterogeneity was evaluated using I-square tests. Five studies comprising 286 patients were analyzed, with 77 tested positive for nasopharyngeal MRSA colonization and 209 tested negative.
Results: MRSA-positive status was significantly associated with a higher rate of PEG-related infection (OR: 24.31, 95% CI [5.20, 113.65], p < 0.0001). Our meta-analysis underscores the notable correlation between nasopharyngeal MRSA colonization and an increased risk of PEG-related infections.
Discussion: These findings emphasize the necessity of factoring in MRSA status when performing PEG insertion procedures. Healthcare providers should remain vigilant in implementing infection prevention strategies, especially in MRSA-positive patients, to reduce complications associated with PEG tube placements. Further investigation is needed to ascertain optimal preventive measures tailored to the MRSA colonization status within this patient cohort.
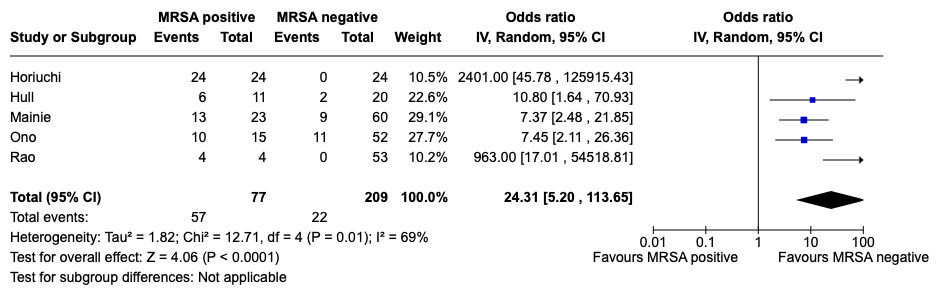
Figure: Forest plot of peristomal wound infection risk
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Islam Mohamed indicated no relevant financial relationships.
Samuel Kim indicated no relevant financial relationships.
Mira Bhatia indicated no relevant financial relationships.
Samiya Azim indicated no relevant financial relationships.
Robert Zhang indicated no relevant financial relationships.
Mira Malavia indicated no relevant financial relationships.
Olivia Sappington indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Syed Hamaad Rahman indicated no relevant financial relationships.
Omar Ahmed indicated no relevant financial relationships.
Islam Mohamed, MD1, Samuel J. Kim, BA2, Mira K. Bhatia, BA1, Samiya Azim, BA1, Robert Zhang, BA3, Mira Malavia, BA1, Olivia Sappington, BA1, Noor Hassan, MD3, Hazem Abosheaishaa, MD4, Dushyant S. Dahiya, MD5, Syed Hamaad Rahman, DO6, Omar T. Ahmed, MD7. P4116 - Nasopharyngeal MRSA Carriage and Risk of PEG-Related Infection: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
