Tuesday Poster Session
Category: General Endoscopy
P4127 - When Vessels Speak: Understanding Aorto-Esophageal Fistula and Its GI Consequences
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NM
Nitish Mittal, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Nitish Mittal, MD, Jimmy Pham, MD, Tanvi Gupta, MD, Jennifer Ma, MD, Nina Quirk, MS, MD, Areeba Khwaja, MD, Chanlir Segarra, MD, Barani Mayilvaganan, MD, FACG
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Aorto-esophageal Fistula (AEF) is an extremely rare but life-threatening and catastrophic cause of upper gastro-intestinal bleeding. Its recognition and diagnosis are challenging and may be delayed with a non-specific presentation to the emergency department. Here, we report a case of an elderly woman who presented with hematemesis, and upper endoscopy showed an ulcer with stigmata of bleeding along with significant extrinsic compression. Further imaging studies revealed presence of an AEF.
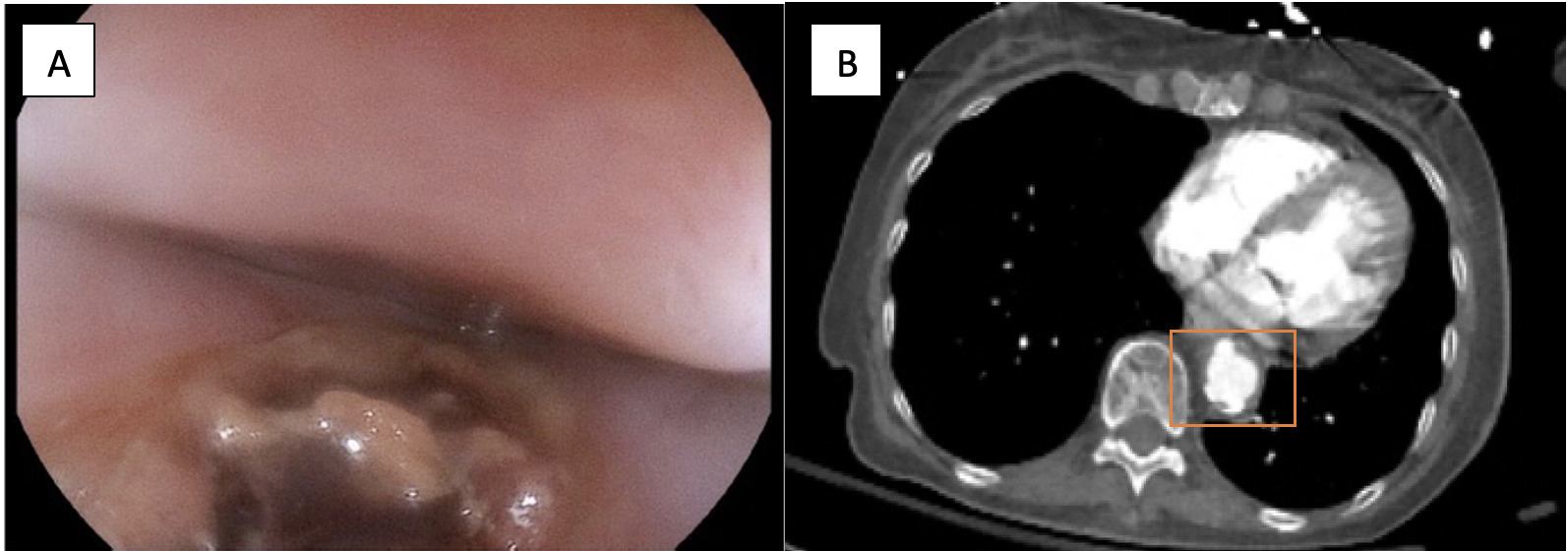
Case Description/Methods: 74-year-old patient who was otherwise healthy apart from hypertension on losartan presented to the hospital after an episode of hematemesis. She was eating some food and vomited bright red blood which prompted her to come to the hospital. She was clinically stable on presentation, and a routine non emergent upper endoscopy was performed. Upper endoscopy revealed a superficial upper esophageal mucosal tear with stigmata of recent bleeding along with suspicion for extrinsic compression over the mid-thoracic esophagus, concerning for possible malignancy causing severe esophageal luminal narrowing (Figure 1A). This area was difficult to evaluate given significant extrinsic compression and 2 cc of 1:10,000 epinephrine was injected given stigmata of bleeding noted at that site. Initial imaging studies suggested questionable compression from possible thoracic/esophageal malignancy and an upper endoscopic ultrasound (EUS) for further evaluation was subsequently planned the following day. Patient had repeated episodes of hematemesis during the night and further CT imaging showed suspicion for aorto-esophageal fistula (Figure 1B). Surgical options were offered, but the patient decided not to proceed with surgery. She was then managed supportively. Although she did not have any bleeding episodes and remained hemodynamically stable for the next 14 hours, she ended up with massive hematemesis the following day and succumbed to death.
Discussion: Our initial suspicion for a life-threatening cause like AEF was low given her clinical presentation and her hemodynamic stability. AEFs can be classified as primary, which directly originate from the native aorta, or secondary, which occur due to prior vascular interventions. Endoscopy plays a significant role in the evaluation but has a poor rate of detection and one should have a high index of suspicion. CT imaging is crucial in making an expedited diagnosis and timely surgical treatment.
Disclosures:
Nitish Mittal, MD, Jimmy Pham, MD, Tanvi Gupta, MD, Jennifer Ma, MD, Nina Quirk, MS, MD, Areeba Khwaja, MD, Chanlir Segarra, MD, Barani Mayilvaganan, MD, FACG. P4127 - When Vessels Speak: Understanding Aorto-Esophageal Fistula and Its GI Consequences, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Aorto-esophageal Fistula (AEF) is an extremely rare but life-threatening and catastrophic cause of upper gastro-intestinal bleeding. Its recognition and diagnosis are challenging and may be delayed with a non-specific presentation to the emergency department. Here, we report a case of an elderly woman who presented with hematemesis, and upper endoscopy showed an ulcer with stigmata of bleeding along with significant extrinsic compression. Further imaging studies revealed presence of an AEF.
Case Description/Methods: 74-year-old patient who was otherwise healthy apart from hypertension on losartan presented to the hospital after an episode of hematemesis. She was eating some food and vomited bright red blood which prompted her to come to the hospital. She was clinically stable on presentation, and a routine non emergent upper endoscopy was performed. Upper endoscopy revealed a superficial upper esophageal mucosal tear with stigmata of recent bleeding along with suspicion for extrinsic compression over the mid-thoracic esophagus, concerning for possible malignancy causing severe esophageal luminal narrowing (Figure 1A). This area was difficult to evaluate given significant extrinsic compression and 2 cc of 1:10,000 epinephrine was injected given stigmata of bleeding noted at that site. Initial imaging studies suggested questionable compression from possible thoracic/esophageal malignancy and an upper endoscopic ultrasound (EUS) for further evaluation was subsequently planned the following day. Patient had repeated episodes of hematemesis during the night and further CT imaging showed suspicion for aorto-esophageal fistula (Figure 1B). Surgical options were offered, but the patient decided not to proceed with surgery. She was then managed supportively. Although she did not have any bleeding episodes and remained hemodynamically stable for the next 14 hours, she ended up with massive hematemesis the following day and succumbed to death.
Discussion: Our initial suspicion for a life-threatening cause like AEF was low given her clinical presentation and her hemodynamic stability. AEFs can be classified as primary, which directly originate from the native aorta, or secondary, which occur due to prior vascular interventions. Endoscopy plays a significant role in the evaluation but has a poor rate of detection and one should have a high index of suspicion. CT imaging is crucial in making an expedited diagnosis and timely surgical treatment.
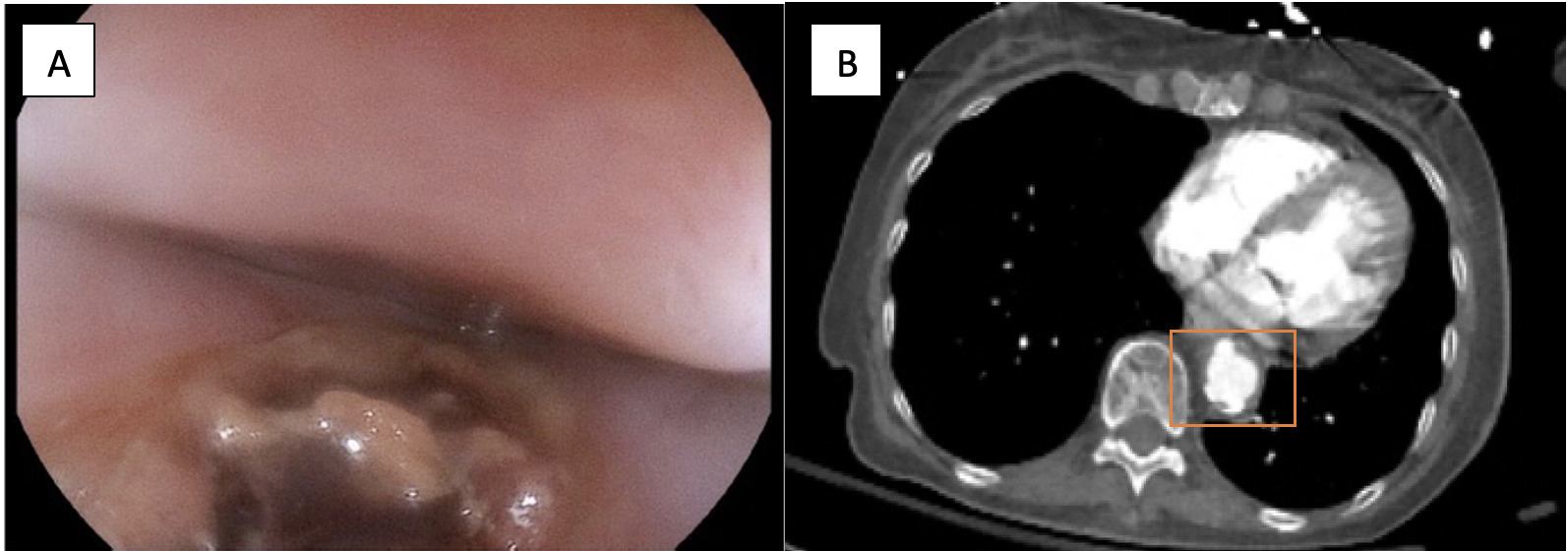
Figure: Figure 1. A: EGD showing upper esophagus mucosal tear; B: CT indicating aortoesophageal fistula (within the orange box – beaking of the aorta)
Disclosures:
Nitish Mittal indicated no relevant financial relationships.
Jimmy Pham indicated no relevant financial relationships.
Tanvi Gupta indicated no relevant financial relationships.
Jennifer Ma indicated no relevant financial relationships.
Nina Quirk indicated no relevant financial relationships.
Areeba Khwaja indicated no relevant financial relationships.
Chanlir Segarra indicated no relevant financial relationships.
Barani Mayilvaganan indicated no relevant financial relationships.
Nitish Mittal, MD, Jimmy Pham, MD, Tanvi Gupta, MD, Jennifer Ma, MD, Nina Quirk, MS, MD, Areeba Khwaja, MD, Chanlir Segarra, MD, Barani Mayilvaganan, MD, FACG. P4127 - When Vessels Speak: Understanding Aorto-Esophageal Fistula and Its GI Consequences, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
