Tuesday Poster Session
Category: General Endoscopy
P4131 - Bleeding Isolated Gastric Varices Secondary to Splenic Vein Thrombosis Successfully Treated With Sclerotherapy Using Ethanolamine Oleate: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Otoniel Hill, MD
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Otoniel Ysea Hill, MD1, Lisa Barrett, DO1, Jordan Carty, MD1, Maria Lagarde Mussa, MD2
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Medical Center, Philadelphia, PA
Introduction: Splenic vein thrombosis (SVT) is a common complication of chronic pancreatitis and pancreatic cancer. Isolated gastric varices (IGV) may develop which have a higher mortality rate than esophageal varices and are more difficult to treat, despite their lower risk of bleeding. In recent years, two widely used first-line treatments for IGV are endoscopic injection sclerotherapy (EIS) using butyl cyanoacrylate (BC) or ethanolamine oleate (EO), and balloon-occluded retrograde transvenous obliteration (B-RTO). Previous studies have concluded that BC is superior to EO, and the survival advantage of BC seems to be partially related to the increased early rebleeding deaths in the EO treated patients. However, BC is not widely available in the US as it is not FDA-approved. Thus, we present a case of a patient with IGV successfully treated with EIS using EO, without rebleeding complications.
Case Description/Methods: A 64-year-old man with history of End Stage Renal Disease status post Kidney Transplant, Renal Artery stenosis status post recent stenting and balloon angioplasty presented to the hospital with a 2-week history of melena and lightheadedness. He had no history of prior GI bleeding or NSAID use. He was on antiplatelet therapy with clopidogrel. He reported daily alcohol use. In the ED, he was normotensive, but tachycardic with HR of 112 bpm. His abdomen was non tender. A digital rectal exam revealed scant melena. Initial labs showed a low Hb of 5.4 g/dl (with a recent baseline of 10 g/dl), INR of 1.2 and a normal platelet count. He was successfully resuscitated and underwent urgent EGD which revealed varices with spurting blood in the gastric fundus (IVG1) that were injected with EO, achieving successful hemostasis. Given no history of cirrhosis and the suspicion of left-sided portal hypertension, he underwent CT abdomen and pelvis that showed chronic SVT and chronic pancreatitis. A transjugular liver biopsy proved low hepatic venous pressure gradient and confirmed no evidence of fibrosis or cirrhosis. The patient subsequently underwent splenectomy for definitive management of his gastric varices, without episodes of rebleeding.
Discussion: We presented a patient with upper gastrointestinal bleeding secondary to IGV1 caused by SVT, who underwent endoscopic treatment with EIS using EO without rebleeding episodes. We demonstrated the safety and efficacy of EO as a sclerosing agent in a patient with unfavorable anatomy for B-RTO.
Disclosures:
Otoniel Ysea Hill, MD1, Lisa Barrett, DO1, Jordan Carty, MD1, Maria Lagarde Mussa, MD2. P4131 - Bleeding Isolated Gastric Varices Secondary to Splenic Vein Thrombosis Successfully Treated With Sclerotherapy Using Ethanolamine Oleate: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Medical Center, Philadelphia, PA
Introduction: Splenic vein thrombosis (SVT) is a common complication of chronic pancreatitis and pancreatic cancer. Isolated gastric varices (IGV) may develop which have a higher mortality rate than esophageal varices and are more difficult to treat, despite their lower risk of bleeding. In recent years, two widely used first-line treatments for IGV are endoscopic injection sclerotherapy (EIS) using butyl cyanoacrylate (BC) or ethanolamine oleate (EO), and balloon-occluded retrograde transvenous obliteration (B-RTO). Previous studies have concluded that BC is superior to EO, and the survival advantage of BC seems to be partially related to the increased early rebleeding deaths in the EO treated patients. However, BC is not widely available in the US as it is not FDA-approved. Thus, we present a case of a patient with IGV successfully treated with EIS using EO, without rebleeding complications.
Case Description/Methods: A 64-year-old man with history of End Stage Renal Disease status post Kidney Transplant, Renal Artery stenosis status post recent stenting and balloon angioplasty presented to the hospital with a 2-week history of melena and lightheadedness. He had no history of prior GI bleeding or NSAID use. He was on antiplatelet therapy with clopidogrel. He reported daily alcohol use. In the ED, he was normotensive, but tachycardic with HR of 112 bpm. His abdomen was non tender. A digital rectal exam revealed scant melena. Initial labs showed a low Hb of 5.4 g/dl (with a recent baseline of 10 g/dl), INR of 1.2 and a normal platelet count. He was successfully resuscitated and underwent urgent EGD which revealed varices with spurting blood in the gastric fundus (IVG1) that were injected with EO, achieving successful hemostasis. Given no history of cirrhosis and the suspicion of left-sided portal hypertension, he underwent CT abdomen and pelvis that showed chronic SVT and chronic pancreatitis. A transjugular liver biopsy proved low hepatic venous pressure gradient and confirmed no evidence of fibrosis or cirrhosis. The patient subsequently underwent splenectomy for definitive management of his gastric varices, without episodes of rebleeding.
Discussion: We presented a patient with upper gastrointestinal bleeding secondary to IGV1 caused by SVT, who underwent endoscopic treatment with EIS using EO without rebleeding episodes. We demonstrated the safety and efficacy of EO as a sclerosing agent in a patient with unfavorable anatomy for B-RTO.
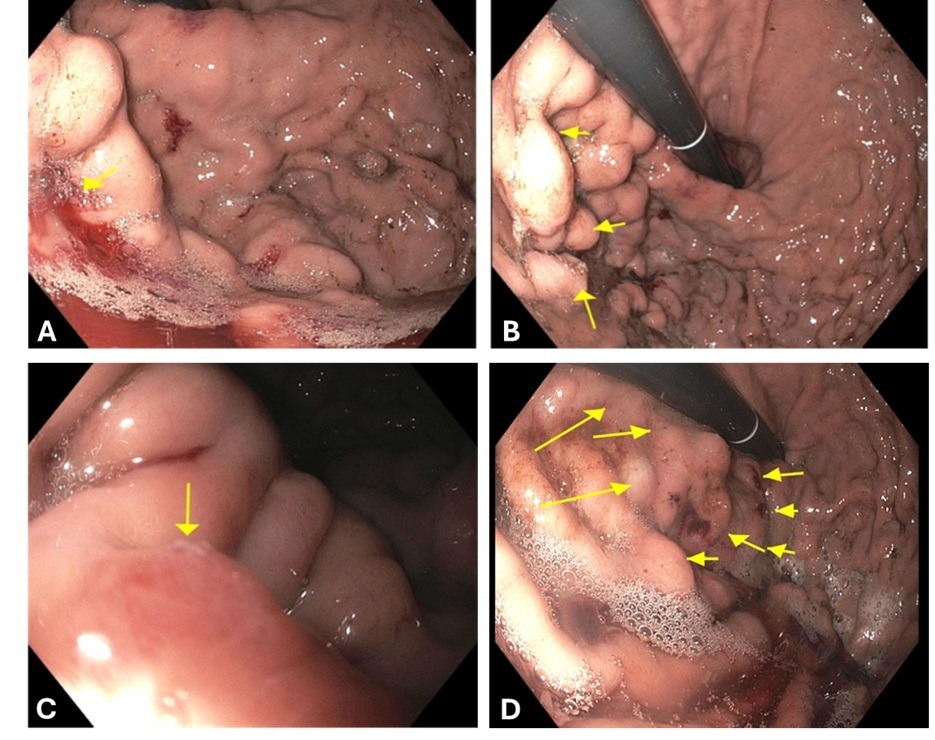
Figure: Upper endoscopy findings:
A) Gastric fundus with active bleeding.
B) Gastric varices (IGV-1).
C) Gastric fundus with “nipple” at the varix.
D) Flattened gastric fundus varices following ethanolamine treatment.
A) Gastric fundus with active bleeding.
B) Gastric varices (IGV-1).
C) Gastric fundus with “nipple” at the varix.
D) Flattened gastric fundus varices following ethanolamine treatment.
Disclosures:
Otoniel Ysea Hill indicated no relevant financial relationships.
Lisa Barrett indicated no relevant financial relationships.
Jordan Carty indicated no relevant financial relationships.
Maria Lagarde Mussa indicated no relevant financial relationships.
Otoniel Ysea Hill, MD1, Lisa Barrett, DO1, Jordan Carty, MD1, Maria Lagarde Mussa, MD2. P4131 - Bleeding Isolated Gastric Varices Secondary to Splenic Vein Thrombosis Successfully Treated With Sclerotherapy Using Ethanolamine Oleate: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
