Tuesday Poster Session
Category: General Endoscopy
P4156 - From Gastroesophageal Reflux to Gastric Pseudomelanosis: A Rare Complication of Chronic Proton Pump Inhibitor Use
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MY
Marcel Yibirin Wakim, MD
Boston Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Leandro Sierra, MD1, Marcel Yibirin, MD2, Marwan Alsaqa, MD3, Carla Barberan Parraga, MD4, Joaquin A.. Calderon, MD5, Iyiad Alabdul Razzak, MD3, Najib Shalabi, MD6, Zoilo K. Suarez, MD7
1Cleveland Clinic Foundation, Cleveland, OH; 2Boston Medical Center, Boston University School of Medicine, Boston, MA; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Maimonides Medical Center, New York, NY; 5George Washington University, Washington, DC; 6Universidad Iberoamericana, Pasadena, CA; 7Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL
Introduction: Pseudomelanosis is an incidental finding often linked to medications and chronic conditions. It presents as brown pigmentation of the intestinal mucosa due to hemosiderin deposits within sub-epithelial macrophages in the lamina propria. It is commonly seen in the duodenum and lower gastrointestinal tract via esophagogastroduodenoscopy (EGD); rare cases have reported malignant melanoma with widespread intestinal melanosis. Due a similar appearance, it is important to biopsy these lesions to exclude this malignancy. We present a case of long-standing gastroesophageal reflux (GERD) resulting in gastric pseudomelanosis, which was identified in the stomach's body and fundus.
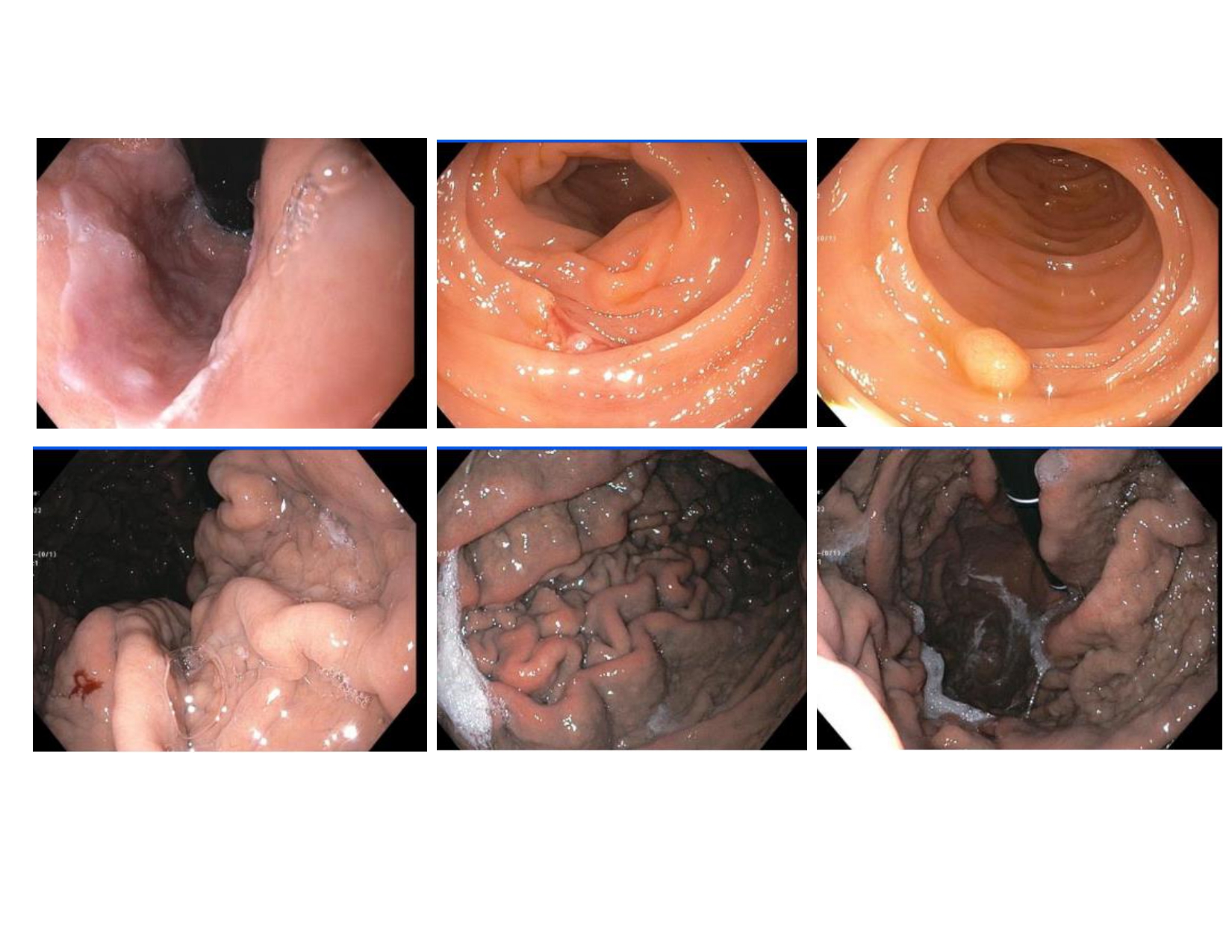
Case Description/Methods: A 72-year-old man with a history of chronic gastroesophageal reflux disease (GERD), colorectal adenomatous polyps, hypertension, and coronary artery disease presented with a two-month history of abdominal bloating and intermittent non-bloody diarrhea. He reported no fever, weight loss, anorexia, abdominal pain, nausea, or vomiting. Given his extensive GERD and colonic polyps history, EGD and colonoscopy were performed. EGD revealed a dark, musky appearance in the gastric body and fundus, prompting a biopsy. The colonoscopy showed multiple tubular polyps, which were removed. Pathology revealed oxyntic mucosa with proton pump inhibitor (PPI) therapy effects and excluded malignancy.
Discussion: Pseudomelanosis, though rare, is a recognized finding in the gastrointestinal tract, mainly in the large and small intestines, especially the duodenum. Literature links these lesions to various medications, including sulfur-containing drugs like pantoprazole, which promote pigment deposition. In our patient, pseudomelanosis was diagnosed due to the absence of malignancy and melanin deposition in biopsy results. Therefore, pseudomelanosis should be considered in patients with GERD on PPI therapy.Although the condition is usually asymptomatic and considered benign, it is important to recognize pseudomelanosis coli during colonoscopy to avoid unnecessary investigations or interventions. The absence of dysplasia, malignancy, or inflammation further supports the benign nature of the condition. The mainstay of management involves discontinuation of anthranoid laxatives if taking any, and the implementation of conservative measures to improve bowel regularity.
Disclosures:
Leandro Sierra, MD1, Marcel Yibirin, MD2, Marwan Alsaqa, MD3, Carla Barberan Parraga, MD4, Joaquin A.. Calderon, MD5, Iyiad Alabdul Razzak, MD3, Najib Shalabi, MD6, Zoilo K. Suarez, MD7. P4156 - From Gastroesophageal Reflux to Gastric Pseudomelanosis: A Rare Complication of Chronic Proton Pump Inhibitor Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Boston Medical Center, Boston University School of Medicine, Boston, MA; 3Beth Israel Deaconess Medical Center, Boston, MA; 4Maimonides Medical Center, New York, NY; 5George Washington University, Washington, DC; 6Universidad Iberoamericana, Pasadena, CA; 7Florida Atlantic University, Charles E. Schmidt College of Medicine, Boca Raton, FL
Introduction: Pseudomelanosis is an incidental finding often linked to medications and chronic conditions. It presents as brown pigmentation of the intestinal mucosa due to hemosiderin deposits within sub-epithelial macrophages in the lamina propria. It is commonly seen in the duodenum and lower gastrointestinal tract via esophagogastroduodenoscopy (EGD); rare cases have reported malignant melanoma with widespread intestinal melanosis. Due a similar appearance, it is important to biopsy these lesions to exclude this malignancy. We present a case of long-standing gastroesophageal reflux (GERD) resulting in gastric pseudomelanosis, which was identified in the stomach's body and fundus.
Case Description/Methods: A 72-year-old man with a history of chronic gastroesophageal reflux disease (GERD), colorectal adenomatous polyps, hypertension, and coronary artery disease presented with a two-month history of abdominal bloating and intermittent non-bloody diarrhea. He reported no fever, weight loss, anorexia, abdominal pain, nausea, or vomiting. Given his extensive GERD and colonic polyps history, EGD and colonoscopy were performed. EGD revealed a dark, musky appearance in the gastric body and fundus, prompting a biopsy. The colonoscopy showed multiple tubular polyps, which were removed. Pathology revealed oxyntic mucosa with proton pump inhibitor (PPI) therapy effects and excluded malignancy.
Discussion: Pseudomelanosis, though rare, is a recognized finding in the gastrointestinal tract, mainly in the large and small intestines, especially the duodenum. Literature links these lesions to various medications, including sulfur-containing drugs like pantoprazole, which promote pigment deposition. In our patient, pseudomelanosis was diagnosed due to the absence of malignancy and melanin deposition in biopsy results. Therefore, pseudomelanosis should be considered in patients with GERD on PPI therapy.Although the condition is usually asymptomatic and considered benign, it is important to recognize pseudomelanosis coli during colonoscopy to avoid unnecessary investigations or interventions. The absence of dysplasia, malignancy, or inflammation further supports the benign nature of the condition. The mainstay of management involves discontinuation of anthranoid laxatives if taking any, and the implementation of conservative measures to improve bowel regularity.
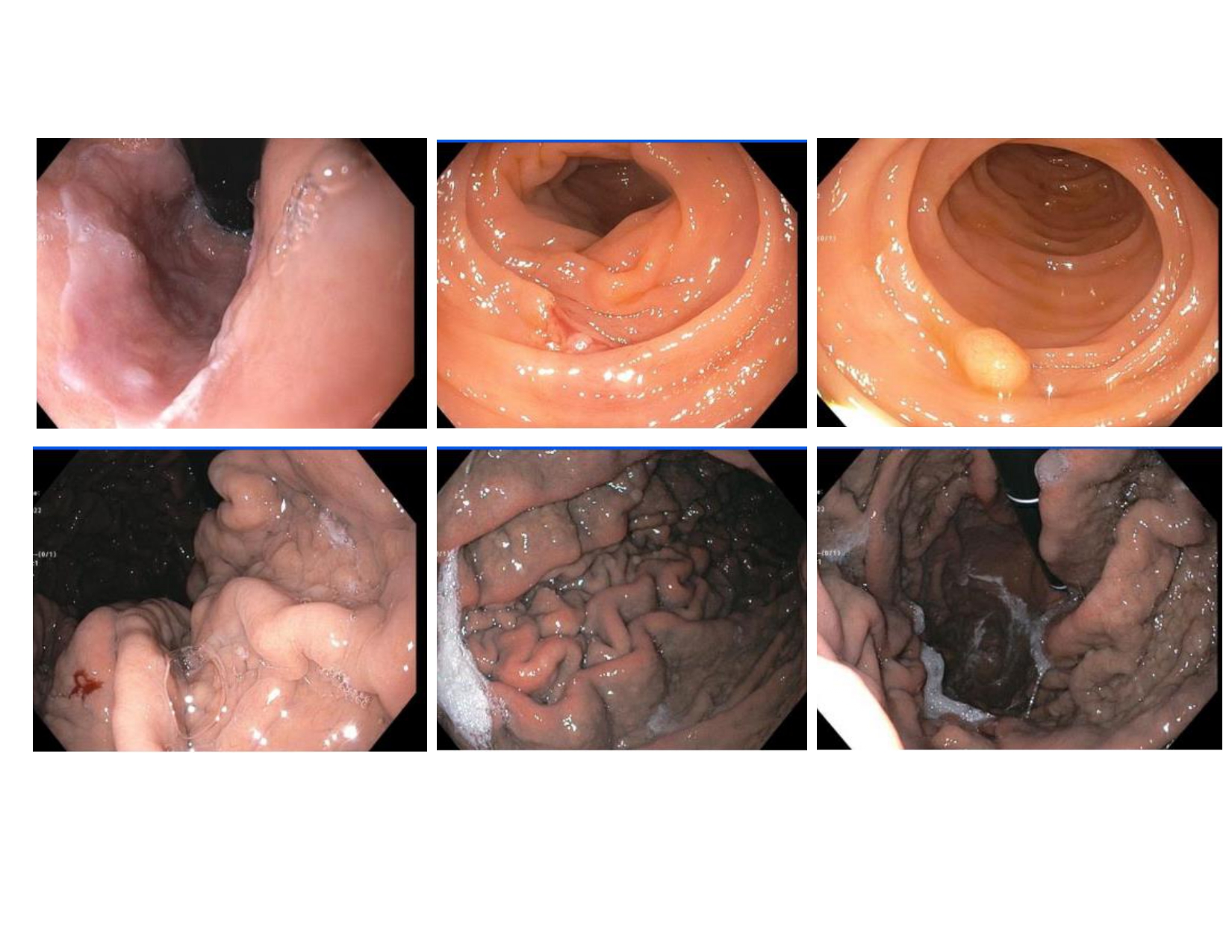
Figure: Esophagogastroduodenoscopy identifying post-GERD polyps and gastric pseudo-melanosis in the body and fundus of the stomach.
Disclosures:
Leandro Sierra indicated no relevant financial relationships.
Marcel Yibirin indicated no relevant financial relationships.
Marwan Alsaqa indicated no relevant financial relationships.
Carla Barberan Parraga indicated no relevant financial relationships.
Joaquin Calderon indicated no relevant financial relationships.
Iyiad Alabdul Razzak indicated no relevant financial relationships.
Najib Shalabi indicated no relevant financial relationships.
Zoilo Suarez indicated no relevant financial relationships.
Leandro Sierra, MD1, Marcel Yibirin, MD2, Marwan Alsaqa, MD3, Carla Barberan Parraga, MD4, Joaquin A.. Calderon, MD5, Iyiad Alabdul Razzak, MD3, Najib Shalabi, MD6, Zoilo K. Suarez, MD7. P4156 - From Gastroesophageal Reflux to Gastric Pseudomelanosis: A Rare Complication of Chronic Proton Pump Inhibitor Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
