Tuesday Poster Session
Category: GI Bleeding
P4158 - Comparison of Prophylactic Transcatheter Arterial Embolization and Standard Therapy in High-Risk Non-Variceal Upper Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SK
Shahryar Khan, MD
University of Kansas
Overland Park, KS
Presenting Author(s)
Shahryar Khan, MD1, Ahmed Khan Jadoon, MD2, Zarlish Rehman, MBBS3, Mashal Alam Khan, MBBS4, Ahmad Khan, MBBS5, Hoor Umar Afridi, MBBS6, Aamer Syed, 7
1University of Kansas, Overland Park, KS; 2The Aga Khan University Hospital, Karachi City, Sindh, Pakistan; 3Hayatabad Medical Complex, Peshawar, North-West Frontier, Pakistan; 4Khyber Medical University, Overland Park, KS; 5Khyber Teaching Hospital, Nowshera, North-West Frontier, Pakistan; 6Khyber Girls Medical College, Peshawar, North-West Frontier, Pakistan; 7Khyber Medical College, Peshawar, North-West Frontier, Pakistan
Introduction: Rebleeding is one of the major challenges and serious complications in non-variceal upper gastrointestinal bleeding (NVUGIB) especially in peptic ulcer disease associated with a higher mortality. Despite Standard Treatment (ST) which includes a combination of Endoscopic therapy and vasoactive drugs, severe rebleeding can happen ultimately requiring Transcatheter arterial embolization (TAE) or Surgery. The prevention of rebleeding is crucial, and empiric TAE has been recommended in patients with a high risk of rebleeding and refractory to endoscopic hemostasis. The aim of the study is to compare the role of prophylactic embolization in preventing the occurrence of NVUGIB as opposed to the standard therapy.
Methods: We systematically searched Medline, and Embase from inception till June 1, 2024. Prophylactic TAE was defined as empirical visceral angiography with no active extravasation and TAE was performed at a high risk of recurrent bleeding. The outcome of interest in our meta-analysis was Rebleeding, while secondary outcomes were All-Cause Mortality, Surgical interventions (SI), Length of Hospital Stay (LOS), and Blood transfusion (BT). The random effects model was used to calculate the Odds ratio (OR), Mean difference (MD) with the corresponding 95% confidence intervals for desired outcomes. Data analysis was performed using the Revman software.
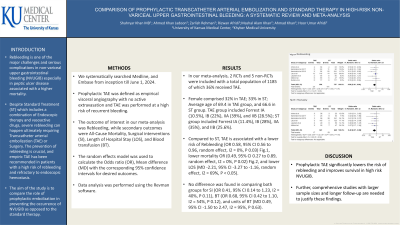
Results: In our meta-analysis, 2 RCTs and 5 non-RCTs were included with a total population of 1185 of which 36% received TAE. Female comprised 32% in TAE; 33% in ST; Average age of 69.4 in TAE group, and 66.6 in ST group. TAE group included Forrest IA (10.5%), IB (22%), IIA (39%), and IIB (28.5%); ST group included Forrest IA (11.4%), IB (28%), IIA (35%), and IIB (25.6%). Compared to ST, TAE is associated with a lower risk of Rebleeding (OR 0.58, 95% CI 0.56 to 0.96, random effect, I2 = 0%, P 0.03) Fig.1, lower mortality OR (0.49, 95% CI 0.27 to 0.89, random effect, I2 = 0%, P 0.02) Fig.2, and lower LOS (MD -2.21, 95% CI -3.27 to -1.16, random effect, I2 = 69%, P < 0.05). No difference was found in comparing both groups for SI (OR 0.41, 95% CI 0.14 to 1.23, I2 = 40%, P 0.11), BT (OR 0.68, 95% CI 0.42 to 1.10, I2 = 54%, P 0.12), and units of BT (MD 0.49, 95% CI -1.50 to 2.47, I2 = 95%, P 0.63).
Discussion: Prophylactic TAE significantly lowers the risk of rebleeding and improves survival in high risk NVUGIB. Further, comprehensive studies with larger sample sizes and longer follow-up are needed to justify these findings.

Disclosures:
Shahryar Khan, MD1, Ahmed Khan Jadoon, MD2, Zarlish Rehman, MBBS3, Mashal Alam Khan, MBBS4, Ahmad Khan, MBBS5, Hoor Umar Afridi, MBBS6, Aamer Syed, 7. P4158 - Comparison of Prophylactic Transcatheter Arterial Embolization and Standard Therapy in High-Risk Non-Variceal Upper Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas, Overland Park, KS; 2The Aga Khan University Hospital, Karachi City, Sindh, Pakistan; 3Hayatabad Medical Complex, Peshawar, North-West Frontier, Pakistan; 4Khyber Medical University, Overland Park, KS; 5Khyber Teaching Hospital, Nowshera, North-West Frontier, Pakistan; 6Khyber Girls Medical College, Peshawar, North-West Frontier, Pakistan; 7Khyber Medical College, Peshawar, North-West Frontier, Pakistan
Introduction: Rebleeding is one of the major challenges and serious complications in non-variceal upper gastrointestinal bleeding (NVUGIB) especially in peptic ulcer disease associated with a higher mortality. Despite Standard Treatment (ST) which includes a combination of Endoscopic therapy and vasoactive drugs, severe rebleeding can happen ultimately requiring Transcatheter arterial embolization (TAE) or Surgery. The prevention of rebleeding is crucial, and empiric TAE has been recommended in patients with a high risk of rebleeding and refractory to endoscopic hemostasis. The aim of the study is to compare the role of prophylactic embolization in preventing the occurrence of NVUGIB as opposed to the standard therapy.
Methods: We systematically searched Medline, and Embase from inception till June 1, 2024. Prophylactic TAE was defined as empirical visceral angiography with no active extravasation and TAE was performed at a high risk of recurrent bleeding. The outcome of interest in our meta-analysis was Rebleeding, while secondary outcomes were All-Cause Mortality, Surgical interventions (SI), Length of Hospital Stay (LOS), and Blood transfusion (BT). The random effects model was used to calculate the Odds ratio (OR), Mean difference (MD) with the corresponding 95% confidence intervals for desired outcomes. Data analysis was performed using the Revman software.
Results: In our meta-analysis, 2 RCTs and 5 non-RCTs were included with a total population of 1185 of which 36% received TAE. Female comprised 32% in TAE; 33% in ST; Average age of 69.4 in TAE group, and 66.6 in ST group. TAE group included Forrest IA (10.5%), IB (22%), IIA (39%), and IIB (28.5%); ST group included Forrest IA (11.4%), IB (28%), IIA (35%), and IIB (25.6%). Compared to ST, TAE is associated with a lower risk of Rebleeding (OR 0.58, 95% CI 0.56 to 0.96, random effect, I2 = 0%, P 0.03) Fig.1, lower mortality OR (0.49, 95% CI 0.27 to 0.89, random effect, I2 = 0%, P 0.02) Fig.2, and lower LOS (MD -2.21, 95% CI -3.27 to -1.16, random effect, I2 = 69%, P < 0.05). No difference was found in comparing both groups for SI (OR 0.41, 95% CI 0.14 to 1.23, I2 = 40%, P 0.11), BT (OR 0.68, 95% CI 0.42 to 1.10, I2 = 54%, P 0.12), and units of BT (MD 0.49, 95% CI -1.50 to 2.47, I2 = 95%, P 0.63).
Discussion: Prophylactic TAE significantly lowers the risk of rebleeding and improves survival in high risk NVUGIB. Further, comprehensive studies with larger sample sizes and longer follow-up are needed to justify these findings.

Figure: Forest plots. Fig.1 and Fig.2
Disclosures:
Shahryar Khan indicated no relevant financial relationships.
Ahmed Khan Jadoon indicated no relevant financial relationships.
Zarlish Rehman indicated no relevant financial relationships.
Mashal Alam Khan indicated no relevant financial relationships.
Ahmad Khan indicated no relevant financial relationships.
Hoor Umar Afridi indicated no relevant financial relationships.
Aamer Syed indicated no relevant financial relationships.
Shahryar Khan, MD1, Ahmed Khan Jadoon, MD2, Zarlish Rehman, MBBS3, Mashal Alam Khan, MBBS4, Ahmad Khan, MBBS5, Hoor Umar Afridi, MBBS6, Aamer Syed, 7. P4158 - Comparison of Prophylactic Transcatheter Arterial Embolization and Standard Therapy in High-Risk Non-Variceal Upper Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
