Tuesday Poster Session
Category: GI Bleeding
P4168 - Early vs Late Bowel Preparation Administration for Suspected Acute Diverticular Bleeds
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Syed Hamaad Rahman, DO
Methodist Dallas Medical Center
Irving, TX
Presenting Author(s)
Syed Hamaad Rahman, DO1, Kyle Schneider, MD2, Hassan Allahrakha, DO3, Juan Carlos Barrera Gutierrez, MD, PhD4, Prashant Kedia, MD, FACG2
1Methodist Dallas Medical Center, Irving, TX; 2Methodist Dallas Medical Center, Dallas, TX; 3Methodist Dallas Medical Center, Allen, TX; 4Methodist Health System, Dallas, TX
Introduction: Diverticular bleeding (DB) is a significant cause of inpatient GI bleeding, with an incidence rate of 30.4 per 100,000 persons in the US. Most cases are self-limited and therapeutic efficacy of colonoscopy for hemostasis is limited. Frequently, bleeding resolves with bowel preparation as old blood is flushed out of the colon. It is useful to understand if bleeding has resolved or is ongoing based on the amount of hematochezia present after bowel preparation. We hypothesized that earlier administration of bowel preparation (< 24 hours) would reduce hospital resource utilization and improve outcomes compared to late administration ( >24 hours).
Methods: We retrospectively identified patients admitted with suspected acute DB from January 2019 to July 2023, excluding patients with secondary diagnoses prolonging hospitalization, other causes of GI bleeding, and diverticulitis. Early bowel preparation (EBP) was given < 24 hours of admission and late bowel preparation (LBP) >24 hours. Variables examined included length of stay, readmissions for GI bleed, RBC transfusions, days to resolution, colonoscopy, hemostasis, hemoglobin levels, tagged RBC scan, and CT angiographies, using Chi-squared and T-tests for statistical analysis.
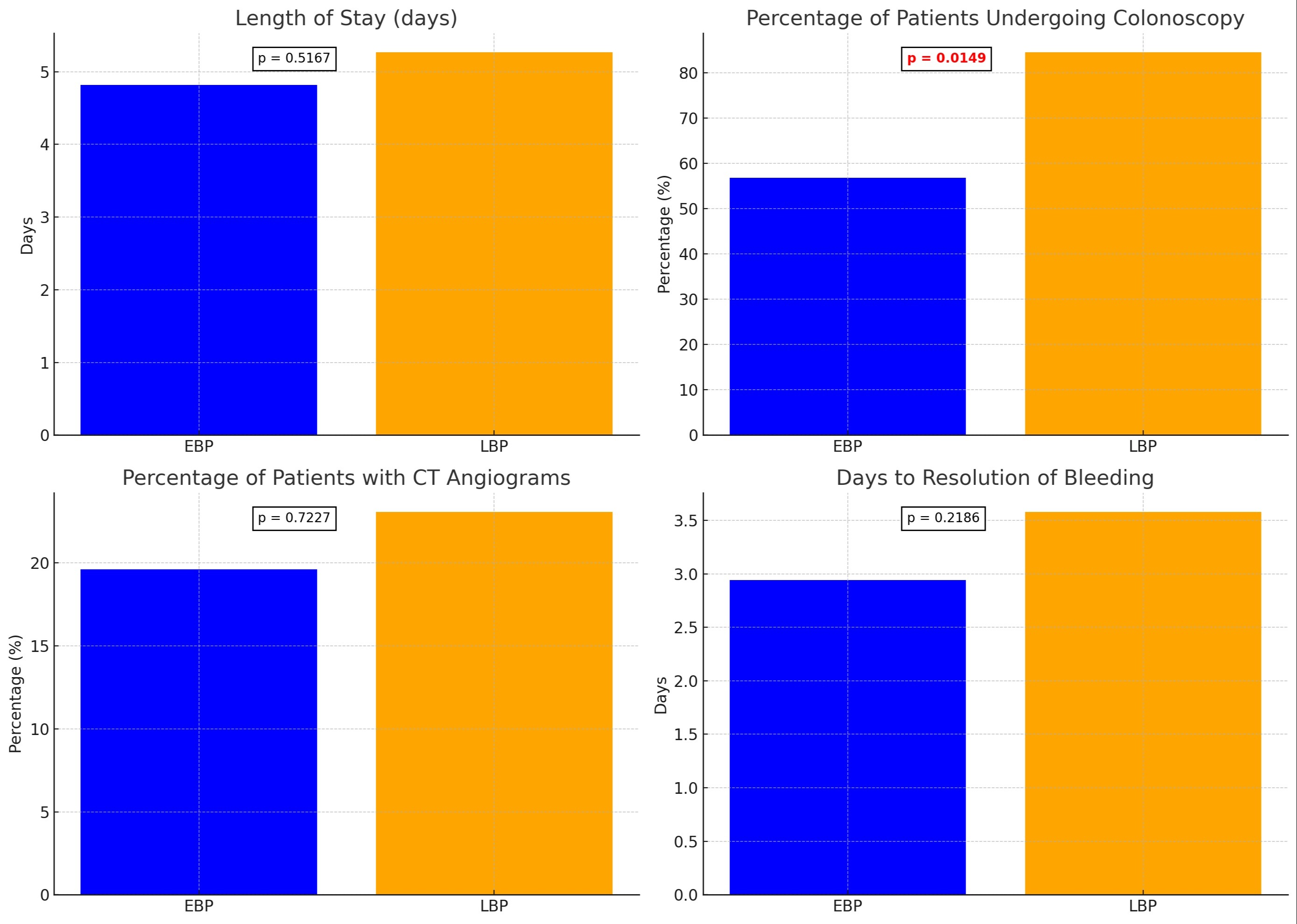
Results: Of 220 patients, 134 met inclusion criteria: EBP (n=51), LBP (n=26), and no bowel preparation (n=57). Baseline characteristics were similar across groups. EBP patients underwent fewer colonoscopies (56.86% vs 84.62%), with statistical significance (p=0.01). EBP group had shorter hospital stays (mean 4.82 vs 5.27 days), faster resolution time (mean 2.94 vs 3.58 days), and fewer CT angiograms (19.61% vs 23.08%), though not statistically significant. EBP patients underwent more tagged RBC scans (37.25% vs 30.77%, p=0.5727). Readmission rates, number of RBC transfusions, hemostasis during colonoscopy, and total imaging orders were similar across groups.
Discussion: EBP compared to LBP for inpatient acute DB was associated with fewer inpatient colonoscopies. There was a trend toward shorter hospital stay, quicker resolution time, and fewer CT angiograms, although these findings were not statistically significant. The significant reduction in colonoscopies in EBP group suggests that EBP may allow clinicians to identify resolved DB quicker and facilitate discharge without unnecessary colonoscopy and other hospital resource utilization. The small sample size of this study is a limitation. Further prospective and randomized trials are needed to confirm these findings.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Syed Hamaad Rahman, DO1, Kyle Schneider, MD2, Hassan Allahrakha, DO3, Juan Carlos Barrera Gutierrez, MD, PhD4, Prashant Kedia, MD, FACG2. P4168 - Early vs Late Bowel Preparation Administration for Suspected Acute Diverticular Bleeds, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Methodist Dallas Medical Center, Irving, TX; 2Methodist Dallas Medical Center, Dallas, TX; 3Methodist Dallas Medical Center, Allen, TX; 4Methodist Health System, Dallas, TX
Introduction: Diverticular bleeding (DB) is a significant cause of inpatient GI bleeding, with an incidence rate of 30.4 per 100,000 persons in the US. Most cases are self-limited and therapeutic efficacy of colonoscopy for hemostasis is limited. Frequently, bleeding resolves with bowel preparation as old blood is flushed out of the colon. It is useful to understand if bleeding has resolved or is ongoing based on the amount of hematochezia present after bowel preparation. We hypothesized that earlier administration of bowel preparation (< 24 hours) would reduce hospital resource utilization and improve outcomes compared to late administration ( >24 hours).
Methods: We retrospectively identified patients admitted with suspected acute DB from January 2019 to July 2023, excluding patients with secondary diagnoses prolonging hospitalization, other causes of GI bleeding, and diverticulitis. Early bowel preparation (EBP) was given < 24 hours of admission and late bowel preparation (LBP) >24 hours. Variables examined included length of stay, readmissions for GI bleed, RBC transfusions, days to resolution, colonoscopy, hemostasis, hemoglobin levels, tagged RBC scan, and CT angiographies, using Chi-squared and T-tests for statistical analysis.
Results: Of 220 patients, 134 met inclusion criteria: EBP (n=51), LBP (n=26), and no bowel preparation (n=57). Baseline characteristics were similar across groups. EBP patients underwent fewer colonoscopies (56.86% vs 84.62%), with statistical significance (p=0.01). EBP group had shorter hospital stays (mean 4.82 vs 5.27 days), faster resolution time (mean 2.94 vs 3.58 days), and fewer CT angiograms (19.61% vs 23.08%), though not statistically significant. EBP patients underwent more tagged RBC scans (37.25% vs 30.77%, p=0.5727). Readmission rates, number of RBC transfusions, hemostasis during colonoscopy, and total imaging orders were similar across groups.
Discussion: EBP compared to LBP for inpatient acute DB was associated with fewer inpatient colonoscopies. There was a trend toward shorter hospital stay, quicker resolution time, and fewer CT angiograms, although these findings were not statistically significant. The significant reduction in colonoscopies in EBP group suggests that EBP may allow clinicians to identify resolved DB quicker and facilitate discharge without unnecessary colonoscopy and other hospital resource utilization. The small sample size of this study is a limitation. Further prospective and randomized trials are needed to confirm these findings.
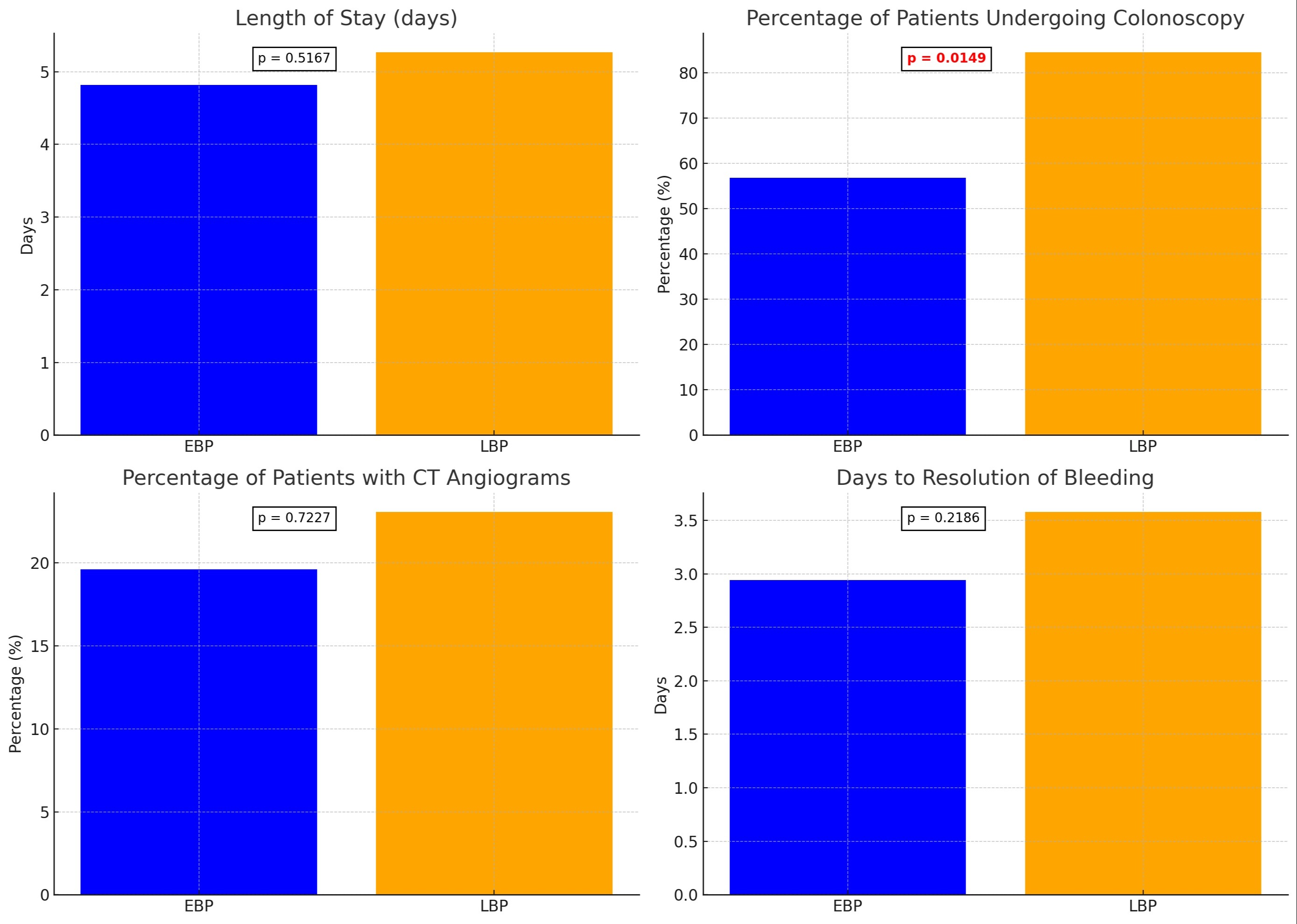
Figure: Graph showing comparative results between EBP and LBP
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Syed Hamaad Rahman indicated no relevant financial relationships.
Kyle Schneider indicated no relevant financial relationships.
Hassan Allahrakha indicated no relevant financial relationships.
Juan Carlos Barrera Gutierrez indicated no relevant financial relationships.
Prashant Kedia: Boston Scientific, Olympus, Medtronic – Consultant.
Syed Hamaad Rahman, DO1, Kyle Schneider, MD2, Hassan Allahrakha, DO3, Juan Carlos Barrera Gutierrez, MD, PhD4, Prashant Kedia, MD, FACG2. P4168 - Early vs Late Bowel Preparation Administration for Suspected Acute Diverticular Bleeds, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
