Tuesday Poster Session
Category: GI Bleeding
P4169 - Are Patient Outcomes Different for Colonoscopic Hemostasis of Stigmata of Hemorrhage Located in the Base vs the Neck of a Diverticulum?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Peerapol Wangrattanapranee, MD
University of Southern California
Granada Hills, CA
Presenting Author(s)
Peerapol Wangrattanapranee, MD1, Dennis Jensen, MD2, Mary Ellen Jensen, 2
1University of Southern California, Granada Hills, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA
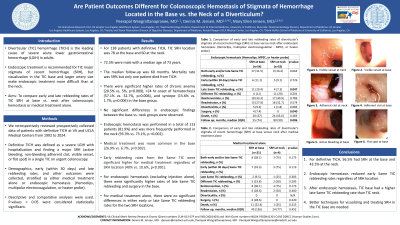
Introduction: Diverticular (TIC) hemorrhage (TICH) is the leading cause of severe acute lower gastrointestinal hemorrhage (LGIH) in adults. Endoscopic treatment is recommended for TIC major stigmata of recent hemorrhage (SRH), but visualization in the TIC base and larger artery size make endoscopic treatment more difficult than at the neck. Aims: To compare early & late rebleeding rates of TIC SRH at base vs. neck after colonoscopic hemostasis or medical treatment alone.
Methods: We retrospectively reviewed prospectively collected data of patients with definitive TICH at VA & UCLA Medical Centers from 1992 to 2024. Definitive TICH was defined as a severe LGIH with hospitalization & finding a major SRH (active bleeding, non-bleeding adherent clot, visible vessel, or flat spot) in a single TIC on urgent colonoscopy. Demographics, early (within 30 days) & late rebleeding rates, and other outcomes were collected, stratified as either medical treatment alone or endoscopic hemostasis (Hemoclips, multipolar electrocoagulation, or heater probe). Descriptive & comparative analyses were used. P-values < 0.05 were considered statistically significant.
Results: For 138 patients with definitive TICH, TIC SRH location was 78 at the base and 60 at the neck. 71.9% were male with a median age of 73 years. The median follow-up was 60 months. Endoscopic hemostasis was performed more often in the neck (93.3% vs. 73.1%, p =0.002), while medical treatment was more common in the base (26.9% vs. 6.7%, p=0.002). Early rebleeding rates from the Same TIC were significant higher for medical treatment regardless of SRH location (40% vs. 10.6%, p< 0.001). No significant differences in demographics & endoscopic findings between the base vs. neck groups were observed. For endoscopic hemostasis (excluding injection alone), there were significantly higher rates of late Same TIC rebleeding and surgery in the base. For medical treatment alone, there were no significant differences in either early or late Same TIC rebleeding rates for the two SRH locations. See Table 1. Mortality rate was 59% but only one patient died from TICH.
Discussion: 1) For definitive TICH, 56.5% had SRH at the base & 43.5% at the neck. 2) Endoscopic hemostasis reduced early Same TIC rebleeding rates regardless of SRH location. 3) After endoscopic hemostasis, TIC base had a higher late Same TIC rebleeding rate than TIC neck. 4) Better techniques for visualizing & treating SRH in the TIC base are needed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Peerapol Wangrattanapranee, MD1, Dennis Jensen, MD2, Mary Ellen Jensen, 2. P4169 - Are Patient Outcomes Different for Colonoscopic Hemostasis of Stigmata of Hemorrhage Located in the Base vs the Neck of a Diverticulum?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Southern California, Granada Hills, CA; 2University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA
Introduction: Diverticular (TIC) hemorrhage (TICH) is the leading cause of severe acute lower gastrointestinal hemorrhage (LGIH) in adults. Endoscopic treatment is recommended for TIC major stigmata of recent hemorrhage (SRH), but visualization in the TIC base and larger artery size make endoscopic treatment more difficult than at the neck. Aims: To compare early & late rebleeding rates of TIC SRH at base vs. neck after colonoscopic hemostasis or medical treatment alone.
Methods: We retrospectively reviewed prospectively collected data of patients with definitive TICH at VA & UCLA Medical Centers from 1992 to 2024. Definitive TICH was defined as a severe LGIH with hospitalization & finding a major SRH (active bleeding, non-bleeding adherent clot, visible vessel, or flat spot) in a single TIC on urgent colonoscopy. Demographics, early (within 30 days) & late rebleeding rates, and other outcomes were collected, stratified as either medical treatment alone or endoscopic hemostasis (Hemoclips, multipolar electrocoagulation, or heater probe). Descriptive & comparative analyses were used. P-values < 0.05 were considered statistically significant.
Results: For 138 patients with definitive TICH, TIC SRH location was 78 at the base and 60 at the neck. 71.9% were male with a median age of 73 years. The median follow-up was 60 months. Endoscopic hemostasis was performed more often in the neck (93.3% vs. 73.1%, p =0.002), while medical treatment was more common in the base (26.9% vs. 6.7%, p=0.002). Early rebleeding rates from the Same TIC were significant higher for medical treatment regardless of SRH location (40% vs. 10.6%, p< 0.001). No significant differences in demographics & endoscopic findings between the base vs. neck groups were observed. For endoscopic hemostasis (excluding injection alone), there were significantly higher rates of late Same TIC rebleeding and surgery in the base. For medical treatment alone, there were no significant differences in either early or late Same TIC rebleeding rates for the two SRH locations. See Table 1. Mortality rate was 59% but only one patient died from TICH.
Discussion: 1) For definitive TICH, 56.5% had SRH at the base & 43.5% at the neck. 2) Endoscopic hemostasis reduced early Same TIC rebleeding rates regardless of SRH location. 3) After endoscopic hemostasis, TIC base had a higher late Same TIC rebleeding rate than TIC neck. 4) Better techniques for visualizing & treating SRH in the TIC base are needed.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Peerapol Wangrattanapranee indicated no relevant financial relationships.
Dennis Jensen indicated no relevant financial relationships.
Mary Ellen Jensen indicated no relevant financial relationships.
Peerapol Wangrattanapranee, MD1, Dennis Jensen, MD2, Mary Ellen Jensen, 2. P4169 - Are Patient Outcomes Different for Colonoscopic Hemostasis of Stigmata of Hemorrhage Located in the Base vs the Neck of a Diverticulum?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

