Tuesday Poster Session
Category: GI Bleeding
P4178 - Intravenous Versus Oral Iron After Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmed Fares, MD
Tufts Medical Center
Boston, MA
Presenting Author(s)
Ahmed Fares, MD1, Mohamed Abuelazm, MD2, Fouad Jaber, MD, MS3, Yazan Sallam, MD3, Mohammad Adam, MD, MSc3, Ahmed Mazen Amin, MBBCh4
1Tufts Medical Center, Boston, MA; 2Tanta University, Tanta, Al Gharbiyah, Egypt; 3University of Missouri - Kansas City School of Medicine, Kansas City, MO; 4Mansoura University, Mansoura, Ad Daqahliyah, Egypt
Introduction: Gastrointestinal bleeding (GIB) is a medical emergency that frequently leads to iron deficiency anemia (IDA). Despite the common use of oral iron supplementation, its gastrointestinal (GI) side effects often result in poor patient compliance. Intravenous (IV) iron offers an alternative with potentially fewer side effects and faster repletion. This study aims to compare the efficacy and safety of IV versus oral iron in treating IDA in patients with GIB.
Methods: A systematic review and meta-analysis were conducted and included randomized controlled trials (RCTs) that compared IV to oral iron supplementation in adult patients with GIB. Databases searched included PubMed, Embase, Cochrane, Scopus, and Web of Science up to April 2024. The primary outcomes were complete response and partial response defined as hemoglobin (Hb) levels ≥12 g/dL, and Hb increase ≥2 g/dL, respectively. Secondary outcomes included Hb change, ferritin change, transferrin saturation (TSAT), and incidence of adverse events. Data were analyzed using fixed-effects models, with results reported as risk ratios (RR) or mean differences (MD) with 95% confidence intervals (CI).
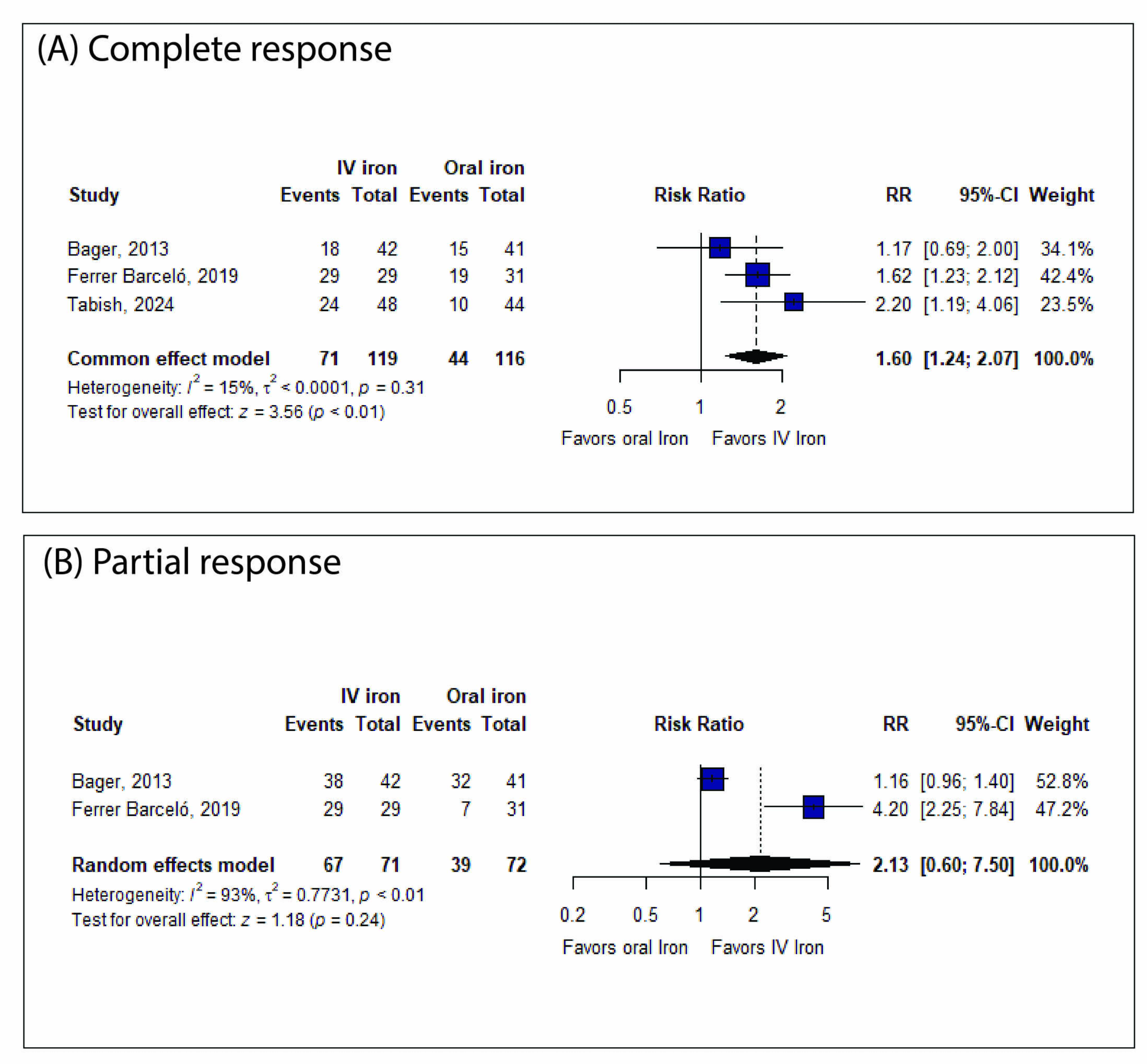
Results: Three RCTs involving 254 patients were included. IV iron significantly increased the complete response rate compared to oral iron (RR: 1.60, 95% CI [1.24, 2.07], P< 0.01; figure 1A). There was no significant difference in partial response (RR: 2.13, 95% CI [0.60, 7.50], P=0.24; figure 1B). IV iron also significantly increased Hb levels (MD: 1.45, 95% CI [0.50, 2.40], P< 0.01; table 1) and ferritin levels (MD: 220.02, 95% CI [22.31, 417.73], P=0.03; table 1). However, no significant difference was found in TSAT (MD: 4.71, 95% CI [-5.96, 15.38], P=0.39; table 1). IV iron was associated with fewer GI adverse events (RR: 0.16 with 95% CI [0.05, 0.52], P< 0.01; table 1) but a higher incidence of hypophosphatemia (RR: 26.68, 95% CI [5.40, 131.79], P< 0.01; table 1).
Discussion: IV iron demonstrated superior efficacy in increasing hemoglobin and ferritin levels and achieving complete response rates in patients with GIB compared to oral iron. This is similar to prior studies that have shown greater efficacy of IV iron compared to oral iron in treating IDA not related to GIB. Despite a higher risk of hypophosphatemia, the reduced incidence of gastrointestinal side effects may improve patient compliance. The findings suggest that IV iron is a viable option for rapid iron repletion in GIB patients and encourages a move to consider first-line treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmed Fares, MD1, Mohamed Abuelazm, MD2, Fouad Jaber, MD, MS3, Yazan Sallam, MD3, Mohammad Adam, MD, MSc3, Ahmed Mazen Amin, MBBCh4. P4178 - Intravenous Versus Oral Iron After Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Tanta University, Tanta, Al Gharbiyah, Egypt; 3University of Missouri - Kansas City School of Medicine, Kansas City, MO; 4Mansoura University, Mansoura, Ad Daqahliyah, Egypt
Introduction: Gastrointestinal bleeding (GIB) is a medical emergency that frequently leads to iron deficiency anemia (IDA). Despite the common use of oral iron supplementation, its gastrointestinal (GI) side effects often result in poor patient compliance. Intravenous (IV) iron offers an alternative with potentially fewer side effects and faster repletion. This study aims to compare the efficacy and safety of IV versus oral iron in treating IDA in patients with GIB.
Methods: A systematic review and meta-analysis were conducted and included randomized controlled trials (RCTs) that compared IV to oral iron supplementation in adult patients with GIB. Databases searched included PubMed, Embase, Cochrane, Scopus, and Web of Science up to April 2024. The primary outcomes were complete response and partial response defined as hemoglobin (Hb) levels ≥12 g/dL, and Hb increase ≥2 g/dL, respectively. Secondary outcomes included Hb change, ferritin change, transferrin saturation (TSAT), and incidence of adverse events. Data were analyzed using fixed-effects models, with results reported as risk ratios (RR) or mean differences (MD) with 95% confidence intervals (CI).
Results: Three RCTs involving 254 patients were included. IV iron significantly increased the complete response rate compared to oral iron (RR: 1.60, 95% CI [1.24, 2.07], P< 0.01; figure 1A). There was no significant difference in partial response (RR: 2.13, 95% CI [0.60, 7.50], P=0.24; figure 1B). IV iron also significantly increased Hb levels (MD: 1.45, 95% CI [0.50, 2.40], P< 0.01; table 1) and ferritin levels (MD: 220.02, 95% CI [22.31, 417.73], P=0.03; table 1). However, no significant difference was found in TSAT (MD: 4.71, 95% CI [-5.96, 15.38], P=0.39; table 1). IV iron was associated with fewer GI adverse events (RR: 0.16 with 95% CI [0.05, 0.52], P< 0.01; table 1) but a higher incidence of hypophosphatemia (RR: 26.68, 95% CI [5.40, 131.79], P< 0.01; table 1).
Discussion: IV iron demonstrated superior efficacy in increasing hemoglobin and ferritin levels and achieving complete response rates in patients with GIB compared to oral iron. This is similar to prior studies that have shown greater efficacy of IV iron compared to oral iron in treating IDA not related to GIB. Despite a higher risk of hypophosphatemia, the reduced incidence of gastrointestinal side effects may improve patient compliance. The findings suggest that IV iron is a viable option for rapid iron repletion in GIB patients and encourages a move to consider first-line treatment.
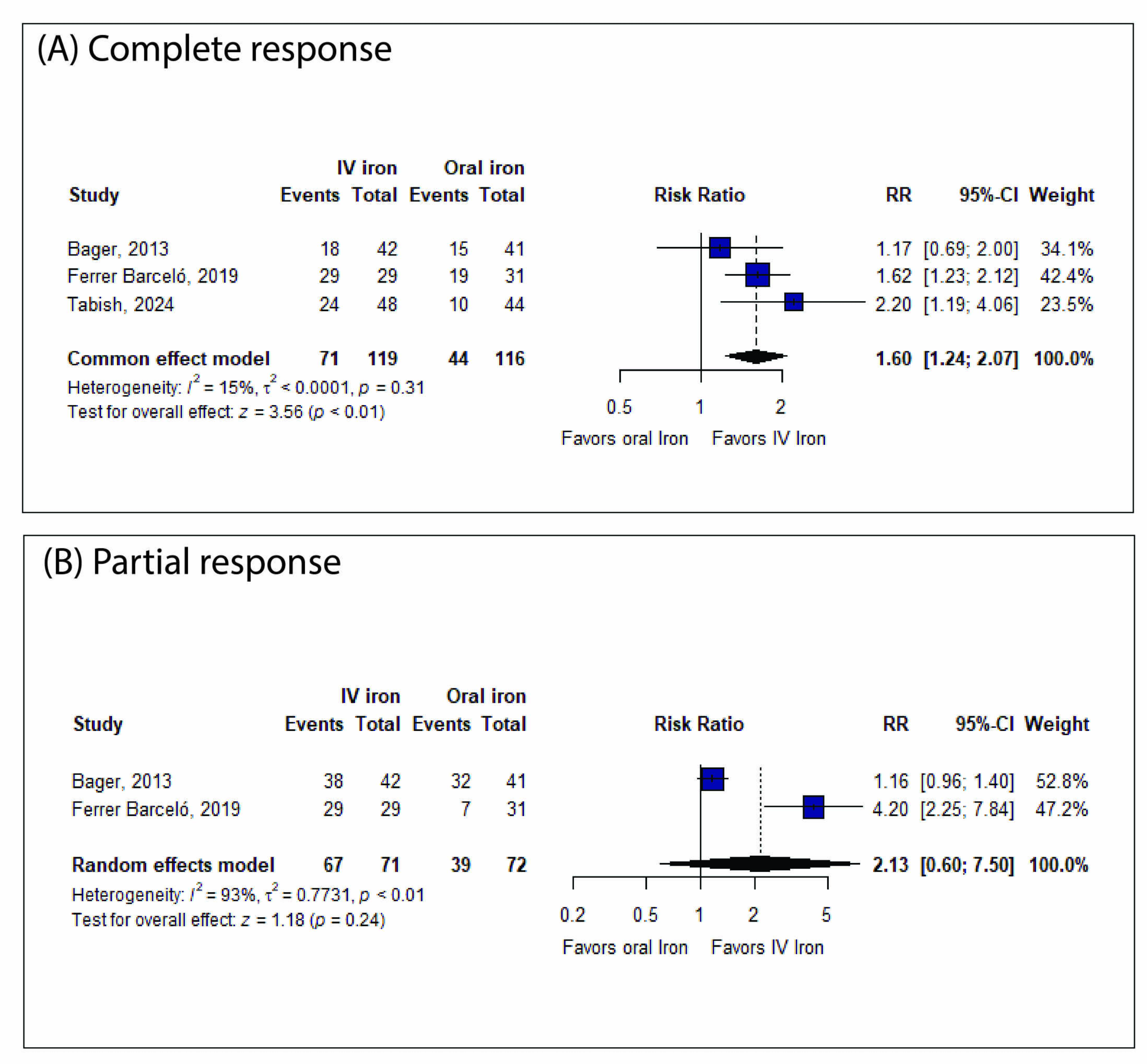
Figure: Figure1: Forest Plots Showing a Comparison of Primary Outcomes
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ahmed Fares indicated no relevant financial relationships.
Mohamed Abuelazm indicated no relevant financial relationships.
Fouad Jaber indicated no relevant financial relationships.
Yazan Sallam indicated no relevant financial relationships.
Mohammad Adam indicated no relevant financial relationships.
Ahmed Mazen Amin indicated no relevant financial relationships.
Ahmed Fares, MD1, Mohamed Abuelazm, MD2, Fouad Jaber, MD, MS3, Yazan Sallam, MD3, Mohammad Adam, MD, MSc3, Ahmed Mazen Amin, MBBCh4. P4178 - Intravenous Versus Oral Iron After Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
