Tuesday Poster Session
Category: GI Bleeding
P4185 - The Impact of Hospital Size on the Outcomes of Patients Admitted with Esophageal Variceal Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- GF
Gianina Flocco, MD
Cleveland Clinic Foundation
Fairview Park, OH
Presenting Author(s)
Gianina Flocco, MD1, Mohamad-Noor Abu-Hammour, MD2, Rashid Abdel-Razeq, MD3, Prabhat Kumar, MD4, Miguel J. Salazar, MD5
1Cleveland Clinic Foundation, Fairview Park, OH; 2Cleveland Clinic Fairview, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5University of California Riverside, Rancho Cucamonga, CA
Introduction: Esophageal variceal bleeding (EBV) is a potentially serious complication of portal hypertension, often causing significant illness and death in patients with cirrhosis. Studies has shown that 25 to 40% of patients with esophageal varices will suffer severe bleeding.
We aim to determine impact of bed size of the admitting institution in outcomes of patients presenting with ( EBV).
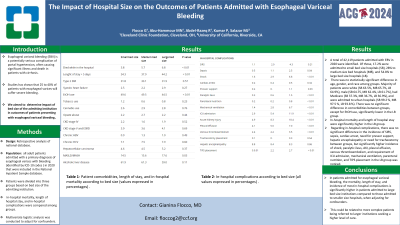
Methods: We conducted a retrospective analysis of all adult patients admitted with a primary diagnosis of esophageal varices with bleeding (identified by ICD-10 codes ) in 2020 that were included in the National Inpatient Sample database.
Patients were divided into three groups based on bed size of the admitting institution. In-hospital mortality, length of hospital stay, and in-hospital complications were compared among groups. Multivariate logistic analysis was conducted to adjust for confounders.
Results: A total of 42,119 patients admitted with EBV in 2020 were identified. Of those, 17.2% were admitted to small bed size hospitals (SB), 28% to medium size bed hospitals (MB), and 54.8% to large bed size hospitals (LB). There was no statistically significant difference in age, gender, and race among groups. Majority of patients were white (SB 63.5%, MB 65.7%, LB 64.9%), male (SB 64.75, MB 62.4%, LB 61.7%), had Medicare (SB 37.3%, MB 36.7%, LB 36.9%), and were admitted to urban hospitals (SB 99.2 %, MB 97.5 %, LB 93.8 %). There was no significant difference in comorbidities between groups, except for EtOH use, significantly lower in the LB group.
In-hospital mortality and length of hospital stay were significantly higher in the LB group. Regarding in-hospital complications, there was no significant difference in the incidence of SIRS, sepsis, cardiac arrest, need for pressor support, hepatic encephalopathy or need for tracheostomy between groups, but significantly higher incidence of shock, paralytic ileus, AKI, pleural effusion, venous thromboembolism, and requirement of ICU admission, mechanical ventilation, parenteral nutrition, and TIPS placement in the LB group was noticed.
Discussion: In patients admitted for esophageal variceal bleeding, the mortality, length of stay, and incidence of most in-hospital complications is significantly higher in patients admitted to large bed size institutions compared to those admitted to smaller size hospitals, when adjusting for confounders. This could be related to more complex patients being referred to larger institutions seeking a higher level of care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gianina Flocco, MD1, Mohamad-Noor Abu-Hammour, MD2, Rashid Abdel-Razeq, MD3, Prabhat Kumar, MD4, Miguel J. Salazar, MD5. P4185 - The Impact of Hospital Size on the Outcomes of Patients Admitted with Esophageal Variceal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Fairview Park, OH; 2Cleveland Clinic Fairview, Cleveland, OH; 3Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Cleveland, OH; 5University of California Riverside, Rancho Cucamonga, CA
Introduction: Esophageal variceal bleeding (EBV) is a potentially serious complication of portal hypertension, often causing significant illness and death in patients with cirrhosis. Studies has shown that 25 to 40% of patients with esophageal varices will suffer severe bleeding.
We aim to determine impact of bed size of the admitting institution in outcomes of patients presenting with ( EBV).
Methods: We conducted a retrospective analysis of all adult patients admitted with a primary diagnosis of esophageal varices with bleeding (identified by ICD-10 codes ) in 2020 that were included in the National Inpatient Sample database.
Patients were divided into three groups based on bed size of the admitting institution. In-hospital mortality, length of hospital stay, and in-hospital complications were compared among groups. Multivariate logistic analysis was conducted to adjust for confounders.
Results: A total of 42,119 patients admitted with EBV in 2020 were identified. Of those, 17.2% were admitted to small bed size hospitals (SB), 28% to medium size bed hospitals (MB), and 54.8% to large bed size hospitals (LB). There was no statistically significant difference in age, gender, and race among groups. Majority of patients were white (SB 63.5%, MB 65.7%, LB 64.9%), male (SB 64.75, MB 62.4%, LB 61.7%), had Medicare (SB 37.3%, MB 36.7%, LB 36.9%), and were admitted to urban hospitals (SB 99.2 %, MB 97.5 %, LB 93.8 %). There was no significant difference in comorbidities between groups, except for EtOH use, significantly lower in the LB group.
In-hospital mortality and length of hospital stay were significantly higher in the LB group. Regarding in-hospital complications, there was no significant difference in the incidence of SIRS, sepsis, cardiac arrest, need for pressor support, hepatic encephalopathy or need for tracheostomy between groups, but significantly higher incidence of shock, paralytic ileus, AKI, pleural effusion, venous thromboembolism, and requirement of ICU admission, mechanical ventilation, parenteral nutrition, and TIPS placement in the LB group was noticed.
Discussion: In patients admitted for esophageal variceal bleeding, the mortality, length of stay, and incidence of most in-hospital complications is significantly higher in patients admitted to large bed size institutions compared to those admitted to smaller size hospitals, when adjusting for confounders. This could be related to more complex patients being referred to larger institutions seeking a higher level of care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Gianina Flocco indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Miguel Salazar indicated no relevant financial relationships.
Gianina Flocco, MD1, Mohamad-Noor Abu-Hammour, MD2, Rashid Abdel-Razeq, MD3, Prabhat Kumar, MD4, Miguel J. Salazar, MD5. P4185 - The Impact of Hospital Size on the Outcomes of Patients Admitted with Esophageal Variceal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
