Tuesday Poster Session
Category: GI Bleeding
P4191 - Strongyloides Associated Gastrointestinal Bleeding in an Immunosuppressed patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Filippa Trikantzopoulou, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Filippa Trikantzopoulou, MD1, Puja Brahmbhatt, MD2, Tanisha Ronnie, MD2, Xianzhong Ding, MD2, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG1
1Loyola University Medical Center, Maywood, IL; 2Loyola University Medical Center, Chicago, IL
Introduction: Strongyloides stercoralis is a parasitic nematode that can cause significant morbidity and mortality, particularly in immunosuppressed individuals. Immunosuppression, often necessary in post-transplant patients to prevent graft rejection, increases the risk of opportunistic infections. We report a case of Strongyloides hyperinfection syndrome leading to gastrointestinal bleeding in an immunosuppressed patient.
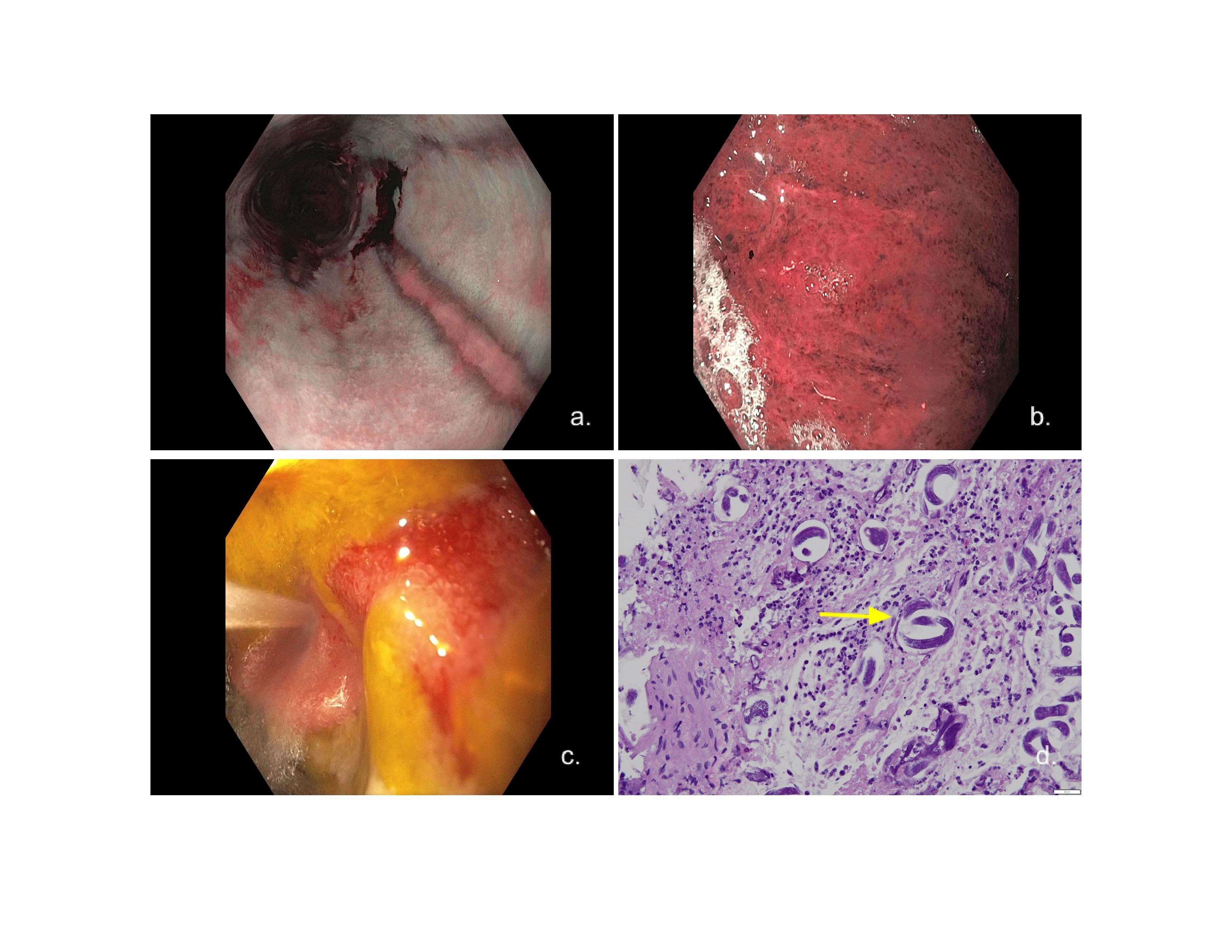
Case Description/Methods: A 70-year-old male from Mexico presented three months post-deceased donor renal transplantation (DDRT) for end stage renal disease (ESRD) of unknown etiology with abdominal pain and concern for small bowel obstruction (SBO) per Computer tomography (CT) findings at outside hospital. Initial imaging (X-ray) was without evidence of obstruction. Despite this, the patient had persistent abdominal pain and new coffee ground emesis. Esophagogastroduodenoscopy (EGD) revealed LA Grade D esophagitis, a linear distal esophageal ulcer, erosive gastropathy, and severe erythematous duodenopathy with contact friability and bleeding (Figure 1a-c). Biopsies were positive for Strongyloides-related active esophagitis and gastritis, as well as duodenitis and ulceration (Figure 1d). He was diagnosed with Strongyloides hyperinfection syndrome. The patient was treated with ivermectin and albendazole. Following, bronchoalvelar lavage showed clearance of the parasite. The patient’s immunosuppressive regimen, which included induction by methylprednisolone and thymoglobulin, followed by daily steroids and myfortic, was held due to septic shock. Despite aggressive treatment, the patient’s condition worsened, with complications of persistent gastrointestinal bleeding, new atrial fibrillation, and concurrent ESBL, MRSA, and Aspergillus fumigatus pneumonias contributing to his death.
Discussion: Strongyloides hyperinfection syndrome can pose a significant risk of gastrointestinal bleeding in immunosuppressed patients. It is crucial to have a high level of suspicion for strongyloidiasis in any patient from an endemic area or with a history of travel to an endemic area, especially if symptoms and blood and/or tissue eosinophilia are present. This case highlights the importance of screening for strongyloidiasis in any patient awaiting transplantation who has epidemiologic risk factors or clinical or laboratory signs of the condition. A multidisciplinary approach and careful management of immunosuppressive therapy are essential to optimizing patient outcomes and preventing fatal complications.
Disclosures:
Filippa Trikantzopoulou, MD1, Puja Brahmbhatt, MD2, Tanisha Ronnie, MD2, Xianzhong Ding, MD2, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG1. P4191 - Strongyloides Associated Gastrointestinal Bleeding in an Immunosuppressed patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Loyola University Medical Center, Maywood, IL; 2Loyola University Medical Center, Chicago, IL
Introduction: Strongyloides stercoralis is a parasitic nematode that can cause significant morbidity and mortality, particularly in immunosuppressed individuals. Immunosuppression, often necessary in post-transplant patients to prevent graft rejection, increases the risk of opportunistic infections. We report a case of Strongyloides hyperinfection syndrome leading to gastrointestinal bleeding in an immunosuppressed patient.
Case Description/Methods: A 70-year-old male from Mexico presented three months post-deceased donor renal transplantation (DDRT) for end stage renal disease (ESRD) of unknown etiology with abdominal pain and concern for small bowel obstruction (SBO) per Computer tomography (CT) findings at outside hospital. Initial imaging (X-ray) was without evidence of obstruction. Despite this, the patient had persistent abdominal pain and new coffee ground emesis. Esophagogastroduodenoscopy (EGD) revealed LA Grade D esophagitis, a linear distal esophageal ulcer, erosive gastropathy, and severe erythematous duodenopathy with contact friability and bleeding (Figure 1a-c). Biopsies were positive for Strongyloides-related active esophagitis and gastritis, as well as duodenitis and ulceration (Figure 1d). He was diagnosed with Strongyloides hyperinfection syndrome. The patient was treated with ivermectin and albendazole. Following, bronchoalvelar lavage showed clearance of the parasite. The patient’s immunosuppressive regimen, which included induction by methylprednisolone and thymoglobulin, followed by daily steroids and myfortic, was held due to septic shock. Despite aggressive treatment, the patient’s condition worsened, with complications of persistent gastrointestinal bleeding, new atrial fibrillation, and concurrent ESBL, MRSA, and Aspergillus fumigatus pneumonias contributing to his death.
Discussion: Strongyloides hyperinfection syndrome can pose a significant risk of gastrointestinal bleeding in immunosuppressed patients. It is crucial to have a high level of suspicion for strongyloidiasis in any patient from an endemic area or with a history of travel to an endemic area, especially if symptoms and blood and/or tissue eosinophilia are present. This case highlights the importance of screening for strongyloidiasis in any patient awaiting transplantation who has epidemiologic risk factors or clinical or laboratory signs of the condition. A multidisciplinary approach and careful management of immunosuppressive therapy are essential to optimizing patient outcomes and preventing fatal complications.
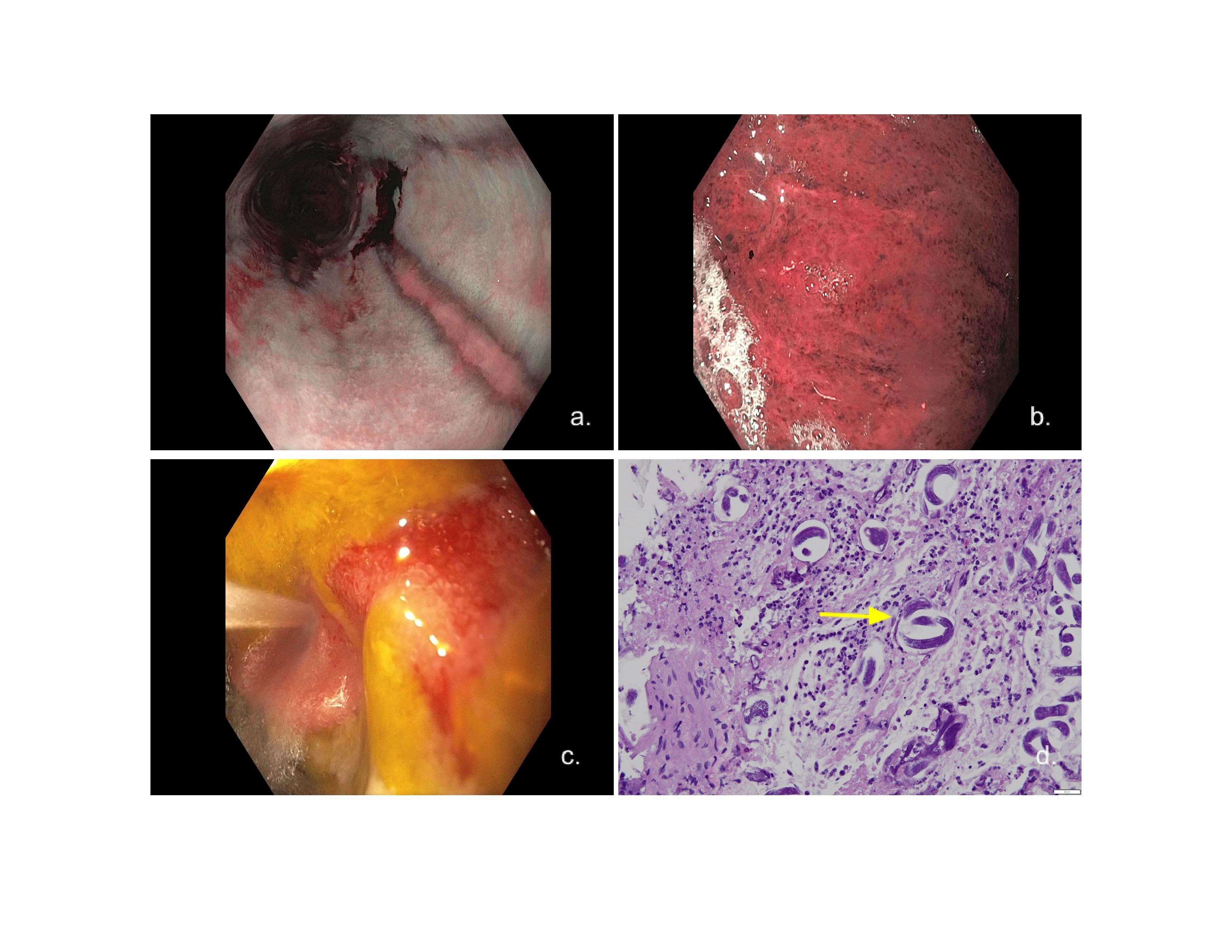
Figure: Figure 1: a. Linear distal esophageal ulcer b. Erosive gastropathy c. Severe duodenopathy with contact friability and bleeding d. Gastric biopsy showcasing strongyloides-related active gastritis (yellow arrow)
Disclosures:
Filippa Trikantzopoulou indicated no relevant financial relationships.
Puja Brahmbhatt indicated no relevant financial relationships.
Tanisha Ronnie indicated no relevant financial relationships.
Xianzhong Ding indicated no relevant financial relationships.
Ayokunle Abegunde: Ferring Pharmaceuticals – Consultant. Ferring Pharmaceuticals – Consultant.
Filippa Trikantzopoulou, MD1, Puja Brahmbhatt, MD2, Tanisha Ronnie, MD2, Xianzhong Ding, MD2, Ayokunle T. Abegunde, MD, MSc, MRCP, FACG1. P4191 - Strongyloides Associated Gastrointestinal Bleeding in an Immunosuppressed patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
