Tuesday Poster Session
Category: GI Bleeding
P4209 - When IBD is Not IBD: A Case of Lymphogranuloma Venereum Proctitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Fnu Vikash, MD, M.Med
Albert Einstein College of Medicine
New York, NY
Presenting Author(s)
Fnu Vikash, MD, M.Med1, Ariel Bar-Mashiah, MD2, Eliza Cricco-Lizza, MD3, Gaurav Ghosh, MD4, Dana J. Lukin, MD5
1Albert Einstein College of Medicine, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 4New York-Presbyterian Hospita/Weill Cornell, New York, NY; 5Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY
Introduction: Lymphogranuloma venereum (LGV) is a sexually transmitted infection caused by the invasive intracellular bacteria Chlamydia trachomatis serovars L1–L3. LGV typically begins with transient, painless genital papules or ulcers, progressing to significant regional lymphadenopathy. While it is a rare cause of proctitis, its clinical presentation can mimic various conditions, making diagnosis challenging (Table 1). Here, we highlight a case that underscores the diagnostic complexities associated with LGV.
Case Description/Methods: A 24-year-old male with no past medical history presented to the ED with lower abdominal pain and bright red blood per rectum (BRBPR) for one month, accompanied by a 15-20 lb weight loss and low-grade fever. He reported tenesmus, urgency, and dyschezia. There was no family history of IBD/CRC
Physical examination revealed suprapubic tenderness and bilateral tender inguinal lymphadenopathy without penile lesions or ulcerations. External anal and digital rectal examinations were unremarkable. Laboratory tests showed anemia with a hemoglobin level of 12 mg/dL and an unremarkable chemistry. Tests for GI PCR, HSV, urine NAAT, and HIV were negative. A CT angiogram of the abdomen and pelvis indicated acute proctitis with perirectal, bilateral inguinal, left external lymphadenopathy and suppurative left inguinal lymphadenopathy.
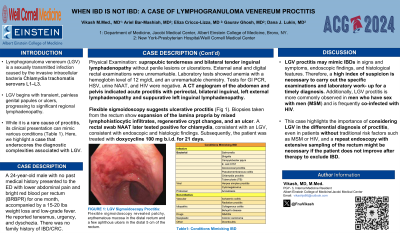
Flexible sigmoidoscopy suggests ulcerative proctitis (Fig 1). Biopsies taken from the rectum show expansion of the lamina propria by mixed lymphohistiocytic infiltrates, regenerative crypt changes, and an ulcer. A rectal swab NAAT later tested positive for chlamydia, consistent with an LGV, consistent with endoscopic and histologic findings. Subsequently, the patient was treated with doxycycline 100 mg b.i.d. for 21 days.
Discussion: LGV proctitis may mimic IBDs in signs and symptoms, endoscopic findings, and histological features. Therefore, a high index of suspicion is necessary to carry out the specific examinations and laboratory work-up for a timely diagnosis. Additionally, LGV proctitis is more commonly observed in men who have sex with men (MSM) and is frequently co-infected with HIV. This case highlights the importance of considering LGV in the differential diagnosis of proctitis, even in patients without traditional risk factors such as MSM or HIV, and a repeat endoscopy with extensive sampling of the rectum might be necessary if the patient does not improve after therapy to exclude IBD.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fnu Vikash, MD, M.Med1, Ariel Bar-Mashiah, MD2, Eliza Cricco-Lizza, MD3, Gaurav Ghosh, MD4, Dana J. Lukin, MD5. P4209 - When IBD is Not IBD: A Case of Lymphogranuloma Venereum Proctitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein College of Medicine, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY; 3New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 4New York-Presbyterian Hospita/Weill Cornell, New York, NY; 5Jill Roberts Center for Inflammatory Bowel Disease, New York Presbyterian Hospital-Weill Cornell Medicine, New York, NY
Introduction: Lymphogranuloma venereum (LGV) is a sexually transmitted infection caused by the invasive intracellular bacteria Chlamydia trachomatis serovars L1–L3. LGV typically begins with transient, painless genital papules or ulcers, progressing to significant regional lymphadenopathy. While it is a rare cause of proctitis, its clinical presentation can mimic various conditions, making diagnosis challenging (Table 1). Here, we highlight a case that underscores the diagnostic complexities associated with LGV.
Case Description/Methods: A 24-year-old male with no past medical history presented to the ED with lower abdominal pain and bright red blood per rectum (BRBPR) for one month, accompanied by a 15-20 lb weight loss and low-grade fever. He reported tenesmus, urgency, and dyschezia. There was no family history of IBD/CRC
Physical examination revealed suprapubic tenderness and bilateral tender inguinal lymphadenopathy without penile lesions or ulcerations. External anal and digital rectal examinations were unremarkable. Laboratory tests showed anemia with a hemoglobin level of 12 mg/dL and an unremarkable chemistry. Tests for GI PCR, HSV, urine NAAT, and HIV were negative. A CT angiogram of the abdomen and pelvis indicated acute proctitis with perirectal, bilateral inguinal, left external lymphadenopathy and suppurative left inguinal lymphadenopathy.
Flexible sigmoidoscopy suggests ulcerative proctitis (Fig 1). Biopsies taken from the rectum show expansion of the lamina propria by mixed lymphohistiocytic infiltrates, regenerative crypt changes, and an ulcer. A rectal swab NAAT later tested positive for chlamydia, consistent with an LGV, consistent with endoscopic and histologic findings. Subsequently, the patient was treated with doxycycline 100 mg b.i.d. for 21 days.
Discussion: LGV proctitis may mimic IBDs in signs and symptoms, endoscopic findings, and histological features. Therefore, a high index of suspicion is necessary to carry out the specific examinations and laboratory work-up for a timely diagnosis. Additionally, LGV proctitis is more commonly observed in men who have sex with men (MSM) and is frequently co-infected with HIV. This case highlights the importance of considering LGV in the differential diagnosis of proctitis, even in patients without traditional risk factors such as MSM or HIV, and a repeat endoscopy with extensive sampling of the rectum might be necessary if the patient does not improve after therapy to exclude IBD.

Figure: Flexible sigmoidoscopy revealed patchy, erythematous mucosa in the distal rectum and a few aphthous ulcers in the distal 5 cm of the rectum with an atypical appearance for ulcerative proctitis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fnu Vikash indicated no relevant financial relationships.
Ariel Bar-Mashiah indicated no relevant financial relationships.
Eliza Cricco-Lizza indicated no relevant financial relationships.
Gaurav Ghosh: Phathom Pharmaceuticals – Consultant.
Dana J. Lukin: AbbVie – Consultant, Grant/Research Support, Speakers Bureau. AltruBio – Consultant. Boehringer Ingelheim – Consultant, Grant/Research Support. Bristol Myers Squibb – Consultant. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Janssen – Consultant, Grant/Research Support, Speakers Bureau. Magellan Health – Consultant. Palatin Technologies – Consultant. Pfizer – Consultant. Prometheus Laboratories – Consultant. PSI – Consultant. Takeda – Consultant, Grant/Research Support.
Fnu Vikash, MD, M.Med1, Ariel Bar-Mashiah, MD2, Eliza Cricco-Lizza, MD3, Gaurav Ghosh, MD4, Dana J. Lukin, MD5. P4209 - When IBD is Not IBD: A Case of Lymphogranuloma Venereum Proctitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

