Tuesday Poster Session
Category: GI Bleeding
P4210 - Challenges in the Management of Upper GI Bleeding in a Patient With Essential Thrombocythemia and Gastroesophageal Varices
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lauren A. Lyssy, DO
The University of Tennessee Health Science Center
Memphis, TN
Presenting Author(s)
Lauren A. Lyssy, DO1, Ryan Mui, DO, PhD2, Jeremy Polman, DO, MS, MBA3
1The University of Tennessee Health Science Center, Memphis, TN; 2Sparrow Hospital, Michigan State University, Okemos, MI; 3Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Essential thrombocythemia (ET) is a myeloproliferative neoplasm (MPN) resulting in excess platelet production. Thrombotic events represent a major cause of morbidity and mortality in these patients. Gastroesophageal varices (GEVs) are a rare complication of ET resulting from portal hypertension secondary to thrombosis. Here, we present a case that highlights the potential challenges of managing upper GI bleeding (UGIB) in a patient with known ET.
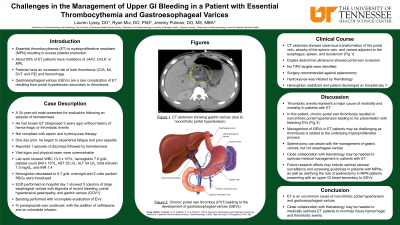
Case Description/Methods: A 34-year-old male presented for evaluation following 1 episode of hematemesis. He had known ET diagnosed 3 years prior but was noncompliant with aspirin and hydroxyurea therapy. He denied any history of thrombotic events or prior GI bleeding. One day before admission, he experienced fatigue and decreased appetite. That morning, he had 1 episode of hematemesis. On admission, vital signs were unremarkable. Lab work showed WBC 10,300, hemoglobin (Hb) 7.8, platelet count 949,000, AST 35, ALT 54, ALP 117, and total bilirubin 1.0. Physical exam was unremarkable. Hemoglobin dropped to 6.7 overnight and 2 units of packed red blood cells were transfused with repeat Hb 7.8. EGD was performed on hospital day 1, showing 5 columns of large ( > 5 mm) esophageal varices with stigmata of recent bleeding, portal hypertensive gastropathy, and gastric varices (GOV1). Banding was performed with incomplete eradication of esophageal varices. IV pantoprazole was continued, and ceftriaxone and an octreotide infusion were started. CT abdomen showed cavernous transformation of the portal vein, atrophy of the splenic vein, and varices adjacent to the esophagus, spleen, and duodenum. Duplex abdominal ultrasound showed portal venous occlusion and splenomegaly. No TIPS targets were identified. Hematology was consulted and hydroxyurea was started. Surgery recommended against splenectomy, which would assist with the management of gastric varices (but not the patient’s bleeding esophageal varices). Hemoglobin remained stable and the patient was discharged on hospital day 7.
Discussion: Management of GEVs in patients with ET may be challenging as thrombosis is related to the underlying myeloproliferative process. Close collaboration with Hematology may be needed to optimize medical management in these patients. Future research efforts may include optimal variceal surveillance and screening guidelines in patients with MPNs as well as to clarify the role of splenectomy in this population when presenting with UGIB secondary to GEVs.
Disclosures:
Lauren A. Lyssy, DO1, Ryan Mui, DO, PhD2, Jeremy Polman, DO, MS, MBA3. P4210 - Challenges in the Management of Upper GI Bleeding in a Patient With Essential Thrombocythemia and Gastroesophageal Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Tennessee Health Science Center, Memphis, TN; 2Sparrow Hospital, Michigan State University, Okemos, MI; 3Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Essential thrombocythemia (ET) is a myeloproliferative neoplasm (MPN) resulting in excess platelet production. Thrombotic events represent a major cause of morbidity and mortality in these patients. Gastroesophageal varices (GEVs) are a rare complication of ET resulting from portal hypertension secondary to thrombosis. Here, we present a case that highlights the potential challenges of managing upper GI bleeding (UGIB) in a patient with known ET.
Case Description/Methods: A 34-year-old male presented for evaluation following 1 episode of hematemesis. He had known ET diagnosed 3 years prior but was noncompliant with aspirin and hydroxyurea therapy. He denied any history of thrombotic events or prior GI bleeding. One day before admission, he experienced fatigue and decreased appetite. That morning, he had 1 episode of hematemesis. On admission, vital signs were unremarkable. Lab work showed WBC 10,300, hemoglobin (Hb) 7.8, platelet count 949,000, AST 35, ALT 54, ALP 117, and total bilirubin 1.0. Physical exam was unremarkable. Hemoglobin dropped to 6.7 overnight and 2 units of packed red blood cells were transfused with repeat Hb 7.8. EGD was performed on hospital day 1, showing 5 columns of large ( > 5 mm) esophageal varices with stigmata of recent bleeding, portal hypertensive gastropathy, and gastric varices (GOV1). Banding was performed with incomplete eradication of esophageal varices. IV pantoprazole was continued, and ceftriaxone and an octreotide infusion were started. CT abdomen showed cavernous transformation of the portal vein, atrophy of the splenic vein, and varices adjacent to the esophagus, spleen, and duodenum. Duplex abdominal ultrasound showed portal venous occlusion and splenomegaly. No TIPS targets were identified. Hematology was consulted and hydroxyurea was started. Surgery recommended against splenectomy, which would assist with the management of gastric varices (but not the patient’s bleeding esophageal varices). Hemoglobin remained stable and the patient was discharged on hospital day 7.
Discussion: Management of GEVs in patients with ET may be challenging as thrombosis is related to the underlying myeloproliferative process. Close collaboration with Hematology may be needed to optimize medical management in these patients. Future research efforts may include optimal variceal surveillance and screening guidelines in patients with MPNs as well as to clarify the role of splenectomy in this population when presenting with UGIB secondary to GEVs.
Disclosures:
Lauren Lyssy indicated no relevant financial relationships.
Ryan Mui indicated no relevant financial relationships.
Jeremy Polman indicated no relevant financial relationships.
Lauren A. Lyssy, DO1, Ryan Mui, DO, PhD2, Jeremy Polman, DO, MS, MBA3. P4210 - Challenges in the Management of Upper GI Bleeding in a Patient With Essential Thrombocythemia and Gastroesophageal Varices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
