Tuesday Poster Session
Category: GI Bleeding
P4236 - Nowhere to Heyde: An Unusual Case of Acquired Coagulopathy-Induced Gastrointestinal Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rahil Desai, DO
Franciscan Health Olympia Fields
Chicago, IL
Presenting Author(s)
Rahil Desai, DO, Shil Punatar, DO, Nabiha Haider, DO, Shyamal Sheth, DO, Vishak Vinod, DO, Sarah Wagmeister, DO, Tilemahos Spyratos, DO
Franciscan Health Olympia Fields, Chicago, IL
Introduction: Heyde syndrome is a rare disorder characterized by a triad of gastrointestinal angiodysplasia or ulcers, acquired von Willebrand syndrome (VS), and aortic stenosis (AS). This exceptionally rare syndrome is noted to be present in 1-3% of patients with AS, and is often diagnosed in patients over age 65. Due to increased circulatory shear forces and cleavage of large Von Willebrand multimers caused by stenosis in the aortic valve (AV), interference with the inhibition of angiogenesis and delivery of clotting factor VIII ensues throughout the body. We present a case of Heyde syndrome with no family history of bleeding disorders. This case is relevant to add to medical literature an uncommon case presentation and subsequent management to allow for prompt and early diagnosis.
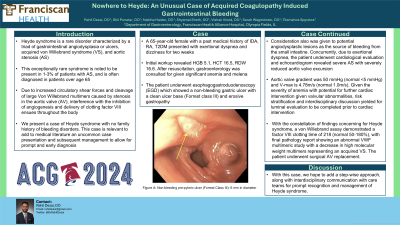
Case Description/Methods: A 65-year-old female with a past medical history of IDA, RA, T2DM presented with exertional dyspnea and dizziness for two weeks. Initial workup revealed HGB 5.1, HCT 16.5, RDW 16.6. After resuscitation, gastroenterology was consulted for given significant anemia and melena. The patient underwent esophagogastroduodenoscopy (EGD) which showed a non-bleeding gastric ulcer with a clean ulcer base (Forrest class III) and erosive gastropathy. Consideration also was given to potential angiodysplastic lesions as the source of bleeding from the small intestine. Concurrently, due to exertional dyspnea, the patient underwent cardiological evaluation and echocardiogram revealed severe AS with severely reduced aortic valve excursion. Aortic valve gradient was 50 mmHg (normal < 5 mmHg) and V-max is 4.78m/s (normal 1.0m/s). Given the severity of anemia with potential for further cardiac intervention given valvular abnormalities, risk stratification and interdisciplinary discussion yielded for luminal evaluation to be completed prior to cardiac intervention. With the constellation of findings concerning for Heyde syndrome, a von Willebrand assay demonstrated a factor VIII clotting time of 218 (normal 50-180%), with final pathology report showing an abnormal VWF multimeric study with a decrease in high molecular weight multimers representing an acquired VS. The patient underwent surgical AV replacement.
Discussion: We highlight an unusual presentation of Heyde syndrome with symptoms of severe anemia, melena, and abnormal clotting studies. With this case, we hope to add a step-wise approach, along with interdisciplinary communication with care teams for prompt recognition and management of Heyde syndrome.

Disclosures:
Rahil Desai, DO, Shil Punatar, DO, Nabiha Haider, DO, Shyamal Sheth, DO, Vishak Vinod, DO, Sarah Wagmeister, DO, Tilemahos Spyratos, DO. P4236 - Nowhere to Heyde: An Unusual Case of Acquired Coagulopathy-Induced Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Franciscan Health Olympia Fields, Chicago, IL
Introduction: Heyde syndrome is a rare disorder characterized by a triad of gastrointestinal angiodysplasia or ulcers, acquired von Willebrand syndrome (VS), and aortic stenosis (AS). This exceptionally rare syndrome is noted to be present in 1-3% of patients with AS, and is often diagnosed in patients over age 65. Due to increased circulatory shear forces and cleavage of large Von Willebrand multimers caused by stenosis in the aortic valve (AV), interference with the inhibition of angiogenesis and delivery of clotting factor VIII ensues throughout the body. We present a case of Heyde syndrome with no family history of bleeding disorders. This case is relevant to add to medical literature an uncommon case presentation and subsequent management to allow for prompt and early diagnosis.
Case Description/Methods: A 65-year-old female with a past medical history of IDA, RA, T2DM presented with exertional dyspnea and dizziness for two weeks. Initial workup revealed HGB 5.1, HCT 16.5, RDW 16.6. After resuscitation, gastroenterology was consulted for given significant anemia and melena. The patient underwent esophagogastroduodenoscopy (EGD) which showed a non-bleeding gastric ulcer with a clean ulcer base (Forrest class III) and erosive gastropathy. Consideration also was given to potential angiodysplastic lesions as the source of bleeding from the small intestine. Concurrently, due to exertional dyspnea, the patient underwent cardiological evaluation and echocardiogram revealed severe AS with severely reduced aortic valve excursion. Aortic valve gradient was 50 mmHg (normal < 5 mmHg) and V-max is 4.78m/s (normal 1.0m/s). Given the severity of anemia with potential for further cardiac intervention given valvular abnormalities, risk stratification and interdisciplinary discussion yielded for luminal evaluation to be completed prior to cardiac intervention. With the constellation of findings concerning for Heyde syndrome, a von Willebrand assay demonstrated a factor VIII clotting time of 218 (normal 50-180%), with final pathology report showing an abnormal VWF multimeric study with a decrease in high molecular weight multimers representing an acquired VS. The patient underwent surgical AV replacement.
Discussion: We highlight an unusual presentation of Heyde syndrome with symptoms of severe anemia, melena, and abnormal clotting studies. With this case, we hope to add a step-wise approach, along with interdisciplinary communication with care teams for prompt recognition and management of Heyde syndrome.

Figure: Non-bleeding pre-pyloric ulcer (Forrest Class III): 6 mm in diameter
Disclosures:
Rahil Desai indicated no relevant financial relationships.
Shil Punatar indicated no relevant financial relationships.
Nabiha Haider indicated no relevant financial relationships.
Shyamal Sheth indicated no relevant financial relationships.
Vishak Vinod indicated no relevant financial relationships.
Sarah Wagmeister indicated no relevant financial relationships.
Tilemahos Spyratos indicated no relevant financial relationships.
Rahil Desai, DO, Shil Punatar, DO, Nabiha Haider, DO, Shyamal Sheth, DO, Vishak Vinod, DO, Sarah Wagmeister, DO, Tilemahos Spyratos, DO. P4236 - Nowhere to Heyde: An Unusual Case of Acquired Coagulopathy-Induced Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
