Tuesday Poster Session
Category: GI Bleeding
P4215 - Gastrointestinal Mucormycosis in an Immunocompetent Host
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Elise Roman, MD
University Hospitals Cleveland Medical Center
Bay Village, OH
Presenting Author(s)
Elise Roman, MD1, Sarah Noble, MD2, Amna Anzar, MD1, Gregory Cooper, MD2
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Gastrointestinal mucormycosis (GIM) is a rare manifestation of mucormycosis in immunocompromised hosts. Cases of GIM, even in the immunocompetent, have been rising (Addasi et al., 2023). GIM may have vague manifestations and early diagnosis and management are critical as it can be rapidly fatal.
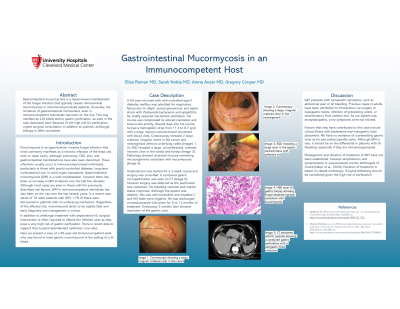
Case Description/Methods: A 65-year-old male with controlled type II diabetes mellitus was admitted for respiratory failure due to Staph. aureus pneumonia, and septic shock with pasteurella bacteremia and epiglottitis. He briefly required mechanical ventilation. His course was complicated by altered mentation and seizure-like activity. Several days into his course, he had a hemoglobin drop from 11.3 to 8.7 with a large, maroon-colored bowel movement with blood clots. Colonoscopy revealed 2 large, cratered, irregular ulcers in the cecum and rectosigmoid without underlying colitis (Images 1, 2). EGD revealed a large, circumferential, cratered, necrotic ulcer in the cardia and fundus (Image 3). Pathology showed ulcerated mucosa containing microorganisms consistent with mucormycosis.
Amphotericin was started for a 2-week course and surgery was consulted. A contained gastric microperforation was seen on CT (Image 4), however surgery was deferred as the perforation was contained. His bleeding resolved and mental status improved. Although the patient was diabetic, this was well-controlled, and hepatitis C and HIV tests were negative. He was discharged on posaconsaole with plans for 6 to 12 months of treatment. Endoscopy 2 months later showed resolution of the gastric ulcer.
Discussion: GIM presents with vague symptoms, such as abdominal pain or GI bleeding. Previous cases in adults have been attributed to introduction via surgery or nasogastric tubes, infection of preexisting ulcers, or dissemination from another site. As our patient was encephalopathic, prior symptoms were not elicited.
Factors that may have contributed to this case include critical illness with bacteremia and nasogastric tube placement. We have no evidence of a preexisting gastric ulcer as he was endoscopically naïve. Although GIM is rare, it should be on the differential in patients with GI bleeding, especially if they are immunosuppressed.
Management and duration of treatment of GIM have not been established, however amphotericin and posaconazole or isavuconazole are the antifungals of choice (Naqvi et al., 2020). Duration of treatment is based on repeat endoscopy. Surgical debulking should be considered given the high risk of perforation.

Disclosures:
Elise Roman, MD1, Sarah Noble, MD2, Amna Anzar, MD1, Gregory Cooper, MD2. P4215 - Gastrointestinal Mucormycosis in an Immunocompetent Host, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Gastrointestinal mucormycosis (GIM) is a rare manifestation of mucormycosis in immunocompromised hosts. Cases of GIM, even in the immunocompetent, have been rising (Addasi et al., 2023). GIM may have vague manifestations and early diagnosis and management are critical as it can be rapidly fatal.
Case Description/Methods: A 65-year-old male with controlled type II diabetes mellitus was admitted for respiratory failure due to Staph. aureus pneumonia, and septic shock with pasteurella bacteremia and epiglottitis. He briefly required mechanical ventilation. His course was complicated by altered mentation and seizure-like activity. Several days into his course, he had a hemoglobin drop from 11.3 to 8.7 with a large, maroon-colored bowel movement with blood clots. Colonoscopy revealed 2 large, cratered, irregular ulcers in the cecum and rectosigmoid without underlying colitis (Images 1, 2). EGD revealed a large, circumferential, cratered, necrotic ulcer in the cardia and fundus (Image 3). Pathology showed ulcerated mucosa containing microorganisms consistent with mucormycosis.
Amphotericin was started for a 2-week course and surgery was consulted. A contained gastric microperforation was seen on CT (Image 4), however surgery was deferred as the perforation was contained. His bleeding resolved and mental status improved. Although the patient was diabetic, this was well-controlled, and hepatitis C and HIV tests were negative. He was discharged on posaconsaole with plans for 6 to 12 months of treatment. Endoscopy 2 months later showed resolution of the gastric ulcer.
Discussion: GIM presents with vague symptoms, such as abdominal pain or GI bleeding. Previous cases in adults have been attributed to introduction via surgery or nasogastric tubes, infection of preexisting ulcers, or dissemination from another site. As our patient was encephalopathic, prior symptoms were not elicited.
Factors that may have contributed to this case include critical illness with bacteremia and nasogastric tube placement. We have no evidence of a preexisting gastric ulcer as he was endoscopically naïve. Although GIM is rare, it should be on the differential in patients with GI bleeding, especially if they are immunosuppressed.
Management and duration of treatment of GIM have not been established, however amphotericin and posaconazole or isavuconazole are the antifungals of choice (Naqvi et al., 2020). Duration of treatment is based on repeat endoscopy. Surgical debulking should be considered given the high risk of perforation.

Figure: Image 1. Colonoscopy showing a large, irregular cratered ulcer in the cecum ; Image 2. Colonoscopy showing a large, irregular, cratered ulcer in the rectosigmoid ; Image 3. EGD revealing a large ulcer in the gastric cardia/fundus with adherent clot ; Image 4: CT abdomen with IV contrast showing a contained gastric perforation with a perigastric fluid collection.
Disclosures:
Elise Roman indicated no relevant financial relationships.
Sarah Noble indicated no relevant financial relationships.
Amna Anzar indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Elise Roman, MD1, Sarah Noble, MD2, Amna Anzar, MD1, Gregory Cooper, MD2. P4215 - Gastrointestinal Mucormycosis in an Immunocompetent Host, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
