Tuesday Poster Session
Category: GI Bleeding
P4218 - Jejunal Diverticular Hemorrhagic Shock: A Case for Enterotomy Over Deep Enteroscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Emilie S. Kim, MD
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Emilie S. Kim, MD1, Ammar Alam, DO1, Daniel Yoon, MD1, Ibrahim Ragab, DO2, Nishit Patel, MD1, Hammad Liaquat, MD1, Noel Martins, MD1
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Allentown, PA
Introduction: Small bowel diverticula are rare causes of diverticular bleeding. In cases where bleeds are challenging to identify, decision algorithms need to be supplemented by timing and severity of the patient's illness. Here, we report a case of hemorrhagic shock caused by a jejunal diverticulum. Our multidisciplinary approach facilitated the prompt identification and expedited treatment of this condition.
Case Description/Methods: A 65-year-old male presented with melena and hematochezia. He required pressors and received over twenty units of blood products. Initial CT angiography (CTA) imaging and endoscopy showed no active bleeding. Push enteroscopy identified clots in duodenal diverticula, fresh blood in the duodenal sweep to proximal jejunum. A Dieulafoy lesion in the gastroesophageal junction was found however patient continued to bleed despite successful treatment, which prompted an inpatient capsule endoscopy. This revealed a suspected active bleed in the jejunum/ileum. Angiogram by interventional radiology (IR) did not identify a source.
The patient deteriorated overnight, with hemodynamic instability and frequent bloody bowel movements. A nuclear bleeding scan was performed, showing uptake in the right upper quadrant. CTA was to confirm active bleeding in a right upper quadrant small bowel loop.
After discussion with gastroenterology, IR and surgery, the patient underwent repeat angiography which was unrevealing and ultimately opted for small bowel enterotomy with enterescopy over a single-balloon enteroscopy. A 100-cm segment with proximal jejunal diverticulosis, containing a culprit diverticulum with fresh clots without oozing, was resected.
Discussion: Multidisciplinary collaboration is crucial in managing hemorrhagic shock from suspected jejunal diverticular bleed. Current literature recommends deep small bowel enteroscopy (single- or double-balloon) for such bleeds in patients without suspected adhesions. However, we saved time by foregoing deep enteroscopy and opting for direct partial small bowel resection. In literature, other cases of massive diverticular hemorrhage managed by surgery with positive outcomes were able to identify the bleeding jejunal diverticulum by CTA, nuclear scan, capsule, or angiogram, however in our case definitive localization was achieved only through intraoperative enteroscopy. Early involvement of IR and surgery is essential to optimize diagnosis and treatment for unstable jejunal diverticular bleeds, regardless of prior surgeries or adhesions.
Disclosures:
Emilie S. Kim, MD1, Ammar Alam, DO1, Daniel Yoon, MD1, Ibrahim Ragab, DO2, Nishit Patel, MD1, Hammad Liaquat, MD1, Noel Martins, MD1. P4218 - Jejunal Diverticular Hemorrhagic Shock: A Case for Enterotomy Over Deep Enteroscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Hospital, Allentown, PA
Introduction: Small bowel diverticula are rare causes of diverticular bleeding. In cases where bleeds are challenging to identify, decision algorithms need to be supplemented by timing and severity of the patient's illness. Here, we report a case of hemorrhagic shock caused by a jejunal diverticulum. Our multidisciplinary approach facilitated the prompt identification and expedited treatment of this condition.
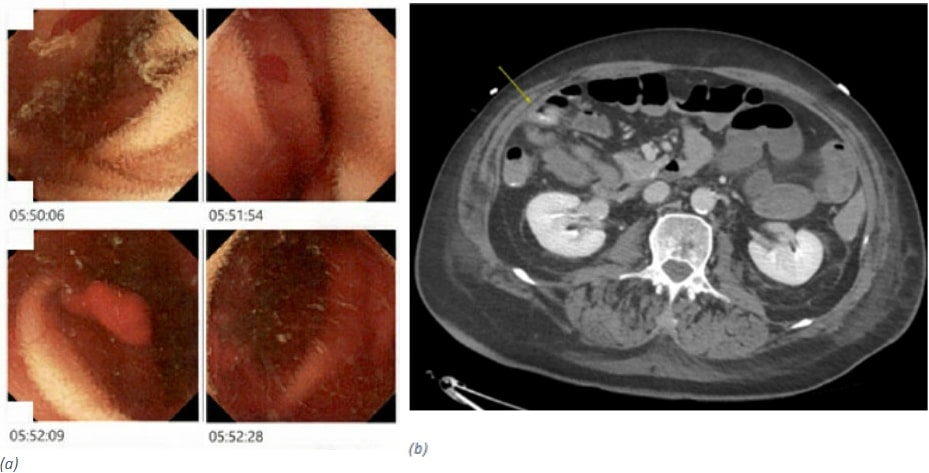
Case Description/Methods: A 65-year-old male presented with melena and hematochezia. He required pressors and received over twenty units of blood products. Initial CT angiography (CTA) imaging and endoscopy showed no active bleeding. Push enteroscopy identified clots in duodenal diverticula, fresh blood in the duodenal sweep to proximal jejunum. A Dieulafoy lesion in the gastroesophageal junction was found however patient continued to bleed despite successful treatment, which prompted an inpatient capsule endoscopy. This revealed a suspected active bleed in the jejunum/ileum. Angiogram by interventional radiology (IR) did not identify a source.
The patient deteriorated overnight, with hemodynamic instability and frequent bloody bowel movements. A nuclear bleeding scan was performed, showing uptake in the right upper quadrant. CTA was to confirm active bleeding in a right upper quadrant small bowel loop.
After discussion with gastroenterology, IR and surgery, the patient underwent repeat angiography which was unrevealing and ultimately opted for small bowel enterotomy with enterescopy over a single-balloon enteroscopy. A 100-cm segment with proximal jejunal diverticulosis, containing a culprit diverticulum with fresh clots without oozing, was resected.
Discussion: Multidisciplinary collaboration is crucial in managing hemorrhagic shock from suspected jejunal diverticular bleed. Current literature recommends deep small bowel enteroscopy (single- or double-balloon) for such bleeds in patients without suspected adhesions. However, we saved time by foregoing deep enteroscopy and opting for direct partial small bowel resection. In literature, other cases of massive diverticular hemorrhage managed by surgery with positive outcomes were able to identify the bleeding jejunal diverticulum by CTA, nuclear scan, capsule, or angiogram, however in our case definitive localization was achieved only through intraoperative enteroscopy. Early involvement of IR and surgery is essential to optimize diagnosis and treatment for unstable jejunal diverticular bleeds, regardless of prior surgeries or adhesions.
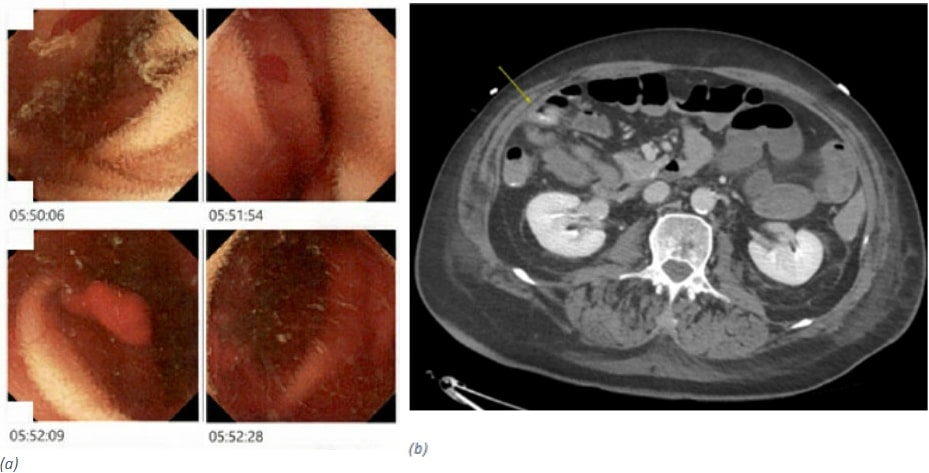
Figure: Figure (a) Capsule endoscopy with oozing starting at suspected small bowel jejunum; (b) CTA right upper quadrant small bowel bleed.
Disclosures:
Emilie S. Kim indicated no relevant financial relationships.
Ammar Alam indicated no relevant financial relationships.
Daniel Yoon indicated no relevant financial relationships.
Ibrahim Ragab indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Hammad Liaquat indicated no relevant financial relationships.
Noel Martins indicated no relevant financial relationships.
Emilie S. Kim, MD1, Ammar Alam, DO1, Daniel Yoon, MD1, Ibrahim Ragab, DO2, Nishit Patel, MD1, Hammad Liaquat, MD1, Noel Martins, MD1. P4218 - Jejunal Diverticular Hemorrhagic Shock: A Case for Enterotomy Over Deep Enteroscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
