Tuesday Poster Session
Category: GI Bleeding
P4223 - An Unexpected Case of Lower GI Bleeding From a Rectal Dieulafoy Lesion
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Gabriel Sperling, MD
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Gabriel Sperling, MD1, Eric Margulies, MD1, Jose Aguirre, MD2
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Galveston,, TX
Introduction: Dieulafoy lesion (DL) is a dilated, aberrant submucosal vessel that erodes the overlying epithelium without a primary ulcer. These lesions are well-recognized but rare, accounting for an estimated 1-2% of all acute GI bleeds. Though they have been found throughout the GI tract, they are typically seen in the stomach (70% of cases) due to its extensive blood supply, with rectal involvement representing just 2% of DL cases. We present a unique case of a significant lower GI bleed (LGIB) due to a rectal DL.
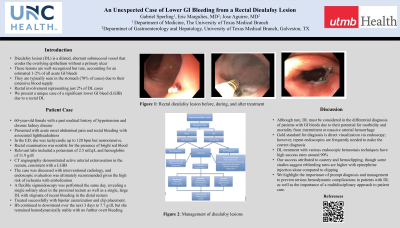
Case Description/Methods: A 60-year-old female with a past medical history of hypertension and chronic kidney disease presented with acute onset abdominal pain and rectal bleeding with associated lightheadedness. In the emergency department, she was tachycardic up to 120 bpm but normotensive. Rectal examination was notable for the presence of bright red blood, and relevant labs included a potassium of 2.5 mEq/L and hemoglobin of 11.9 g/dl. CT angiography demonstrated active arterial extravasation in the rectum, consistent with a LGIB. The case was discussed with interventional radiology, and endoscopic evaluation was ultimately recommended given the high risk of ischemia with embolization. A flexible sigmoidoscopy was performed the same day, revealing a single solitary ulcer in the proximal rectum as well as a single, large DL with stigmata of recent bleeding in the distal rectum. This lesion was treated successfully with bipolar cauterization and clip placement. The hemoglobin continued to downtrend over the next 3 days to 7.7 g/dl, but she remained hemodynamically stable with no further overt bleeding and was safely discharged with close GI follow-up.
Discussion: Although rare, DL must be considered in the differential diagnosis of patients with GI bleeds due to their potential for morbidity and mortality from intermittent or massive arterial hemorrhage. The gold standard for diagnosis is direct visualization via endoscopy; however, repeat endoscopies are frequently needed to make the correct diagnosis. DL treatment with various endoscopic hemostasis techniques have high success rates around 90%, with our success attributed to cautery and hemoclipping, though some studies suggest rebleeding rates are higher with epinephrine injection alone compared to clipping. We highlight the importance of prompt diagnosis and management to prevent serious hemodynamic complications in patients with DL as well as the importance of a multidisciplinary approach to patient care.

Disclosures:
Gabriel Sperling, MD1, Eric Margulies, MD1, Jose Aguirre, MD2. P4223 - An Unexpected Case of Lower GI Bleeding From a Rectal Dieulafoy Lesion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2University of Texas Medical Branch, Galveston,, TX
Introduction: Dieulafoy lesion (DL) is a dilated, aberrant submucosal vessel that erodes the overlying epithelium without a primary ulcer. These lesions are well-recognized but rare, accounting for an estimated 1-2% of all acute GI bleeds. Though they have been found throughout the GI tract, they are typically seen in the stomach (70% of cases) due to its extensive blood supply, with rectal involvement representing just 2% of DL cases. We present a unique case of a significant lower GI bleed (LGIB) due to a rectal DL.
Case Description/Methods: A 60-year-old female with a past medical history of hypertension and chronic kidney disease presented with acute onset abdominal pain and rectal bleeding with associated lightheadedness. In the emergency department, she was tachycardic up to 120 bpm but normotensive. Rectal examination was notable for the presence of bright red blood, and relevant labs included a potassium of 2.5 mEq/L and hemoglobin of 11.9 g/dl. CT angiography demonstrated active arterial extravasation in the rectum, consistent with a LGIB. The case was discussed with interventional radiology, and endoscopic evaluation was ultimately recommended given the high risk of ischemia with embolization. A flexible sigmoidoscopy was performed the same day, revealing a single solitary ulcer in the proximal rectum as well as a single, large DL with stigmata of recent bleeding in the distal rectum. This lesion was treated successfully with bipolar cauterization and clip placement. The hemoglobin continued to downtrend over the next 3 days to 7.7 g/dl, but she remained hemodynamically stable with no further overt bleeding and was safely discharged with close GI follow-up.
Discussion: Although rare, DL must be considered in the differential diagnosis of patients with GI bleeds due to their potential for morbidity and mortality from intermittent or massive arterial hemorrhage. The gold standard for diagnosis is direct visualization via endoscopy; however, repeat endoscopies are frequently needed to make the correct diagnosis. DL treatment with various endoscopic hemostasis techniques have high success rates around 90%, with our success attributed to cautery and hemoclipping, though some studies suggest rebleeding rates are higher with epinephrine injection alone compared to clipping. We highlight the importance of prompt diagnosis and management to prevent serious hemodynamic complications in patients with DL as well as the importance of a multidisciplinary approach to patient care.

Figure: Figure 1: Rectal dieulafoy lesion before, during, and after treatment
Disclosures:
Gabriel Sperling indicated no relevant financial relationships.
Eric Margulies indicated no relevant financial relationships.
Jose Aguirre indicated no relevant financial relationships.
Gabriel Sperling, MD1, Eric Margulies, MD1, Jose Aguirre, MD2. P4223 - An Unexpected Case of Lower GI Bleeding From a Rectal Dieulafoy Lesion, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
