Tuesday Poster Session
Category: GI Bleeding
P4227 - Bleeding in the Shadows: Isolated Jejunal Varices Treated with Push Enteroscopy Sclerotherapy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JK
Jagadish Koyi, MD
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Award: Presidential Poster Award
Jagadish Koyi, MD1, Mir Zulqarnain, DO2, Mohamed Ahmed, MD3, Anand Venugopal, MD, PhD4, Wendell Clarkston, MD5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO; 3University of Missouri-Kansas City, Saint Luke's Hospital, Kansas City, MO; 4University of Missouri Kansas City School of Medicine, Saint Lukes Hospital, Kansas City, MO; 5University of Missouri - Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO
Introduction: Small Intestinal varices account for < 5% gastrointestinal bleeding (GIB) and most often are secondary to prior abdominal surgeries or portal hypertension. Here we present a rare case of massive GIB due to isolated jejunal varices in the absence of overt signs of portal hypertension or prior abdominal surgeries.
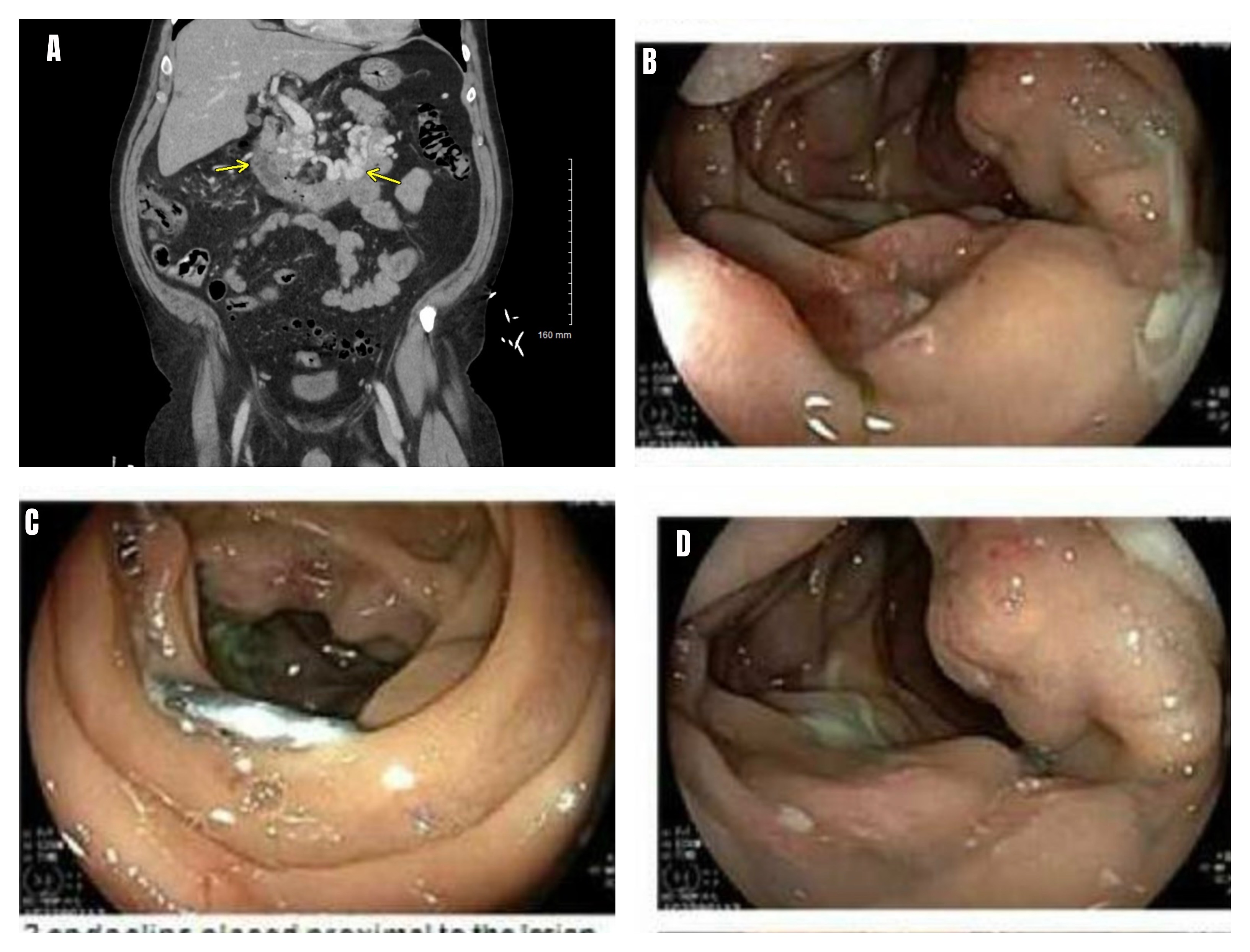
Case Description/Methods: A 62-year-old male with atrial fibrillation, chronic alcohol use presented with melena. Initial vitals were 80/40mm Hg with labs noting hemoglobin 4.6g/dl. Patient was resuscitated with blood products. Imaging with computed tomography with angiography revealed dilated varicose veins in walls of the proximal jejunum and infiltration of mesenteric fat with mesenteric adenopathy along with bilateral pulmonary emboli (PE). Push enteroscopy revealed multiple proximal jejunal varices with stigmata of recent bleeding from about 105cm to 115 cm of scope insertion. Endoclips were placed for localization. MRI abdomen revealed isolated superior mesenteric vein thrombosis (SMV) as a likely cause of jejunal varices. IR was unsuccessful at SMV recanalization. There was concern for infiltrative or malignant process in the mesentery causing occlusion of SMV. Oncology work up revealed mildly reduced protein C level (61%) with hypercellular bone marrow. Liver biopsy revealed steatohepatitis and fibrosis (stage 2-3), and mesenteric lymph node biopsy was negative for malignancy. Patient was discharged with anticoagulation for PE but was readmitted with recurrent melena. Repeat push enteroscopy revealed three columns of jejunal varices seen adjacent to a previously placed Endo Clip with one column appearing to have multiple areas of red nipple sign and red wale sign with active oozing. Due to active bleeding, this column was injected with 4 ml of sclerosing agent with adequate hemostasis.
Discussion: The management of ectopic varices associated with cirrhosis, portal hypertension is well defined and includes treatment modalities such as octreotide, beta-blockers, Transjugular Intrahepatic Portosystemic Shunts, etc. However the optimal management of isolated ectopic varices without cirrhosis is less clear. There are only a few case reports applying sclerotherapy for the treatment of isolated jejunal varices. Three recent cases reported sclerotherapy for jejunal varices at the site of choledochojejunostomy and one case utilized double balloon enteroscopy with sclerotherapy. This case adds to this limited literature regarding the safety and efficacy of small volume sclerotherapy.
Disclosures:
Jagadish Koyi, MD1, Mir Zulqarnain, DO2, Mohamed Ahmed, MD3, Anand Venugopal, MD, PhD4, Wendell Clarkston, MD5. P4227 - Bleeding in the Shadows: Isolated Jejunal Varices Treated with Push Enteroscopy Sclerotherapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jagadish Koyi, MD1, Mir Zulqarnain, DO2, Mohamed Ahmed, MD3, Anand Venugopal, MD, PhD4, Wendell Clarkston, MD5
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO; 3University of Missouri-Kansas City, Saint Luke's Hospital, Kansas City, MO; 4University of Missouri Kansas City School of Medicine, Saint Lukes Hospital, Kansas City, MO; 5University of Missouri - Kansas City School of Medicine, Saint Luke's Hospital, Kansas City, MO
Introduction: Small Intestinal varices account for < 5% gastrointestinal bleeding (GIB) and most often are secondary to prior abdominal surgeries or portal hypertension. Here we present a rare case of massive GIB due to isolated jejunal varices in the absence of overt signs of portal hypertension or prior abdominal surgeries.
Case Description/Methods: A 62-year-old male with atrial fibrillation, chronic alcohol use presented with melena. Initial vitals were 80/40mm Hg with labs noting hemoglobin 4.6g/dl. Patient was resuscitated with blood products. Imaging with computed tomography with angiography revealed dilated varicose veins in walls of the proximal jejunum and infiltration of mesenteric fat with mesenteric adenopathy along with bilateral pulmonary emboli (PE). Push enteroscopy revealed multiple proximal jejunal varices with stigmata of recent bleeding from about 105cm to 115 cm of scope insertion. Endoclips were placed for localization. MRI abdomen revealed isolated superior mesenteric vein thrombosis (SMV) as a likely cause of jejunal varices. IR was unsuccessful at SMV recanalization. There was concern for infiltrative or malignant process in the mesentery causing occlusion of SMV. Oncology work up revealed mildly reduced protein C level (61%) with hypercellular bone marrow. Liver biopsy revealed steatohepatitis and fibrosis (stage 2-3), and mesenteric lymph node biopsy was negative for malignancy. Patient was discharged with anticoagulation for PE but was readmitted with recurrent melena. Repeat push enteroscopy revealed three columns of jejunal varices seen adjacent to a previously placed Endo Clip with one column appearing to have multiple areas of red nipple sign and red wale sign with active oozing. Due to active bleeding, this column was injected with 4 ml of sclerosing agent with adequate hemostasis.
Discussion: The management of ectopic varices associated with cirrhosis, portal hypertension is well defined and includes treatment modalities such as octreotide, beta-blockers, Transjugular Intrahepatic Portosystemic Shunts, etc. However the optimal management of isolated ectopic varices without cirrhosis is less clear. There are only a few case reports applying sclerotherapy for the treatment of isolated jejunal varices. Three recent cases reported sclerotherapy for jejunal varices at the site of choledochojejunostomy and one case utilized double balloon enteroscopy with sclerotherapy. This case adds to this limited literature regarding the safety and efficacy of small volume sclerotherapy.
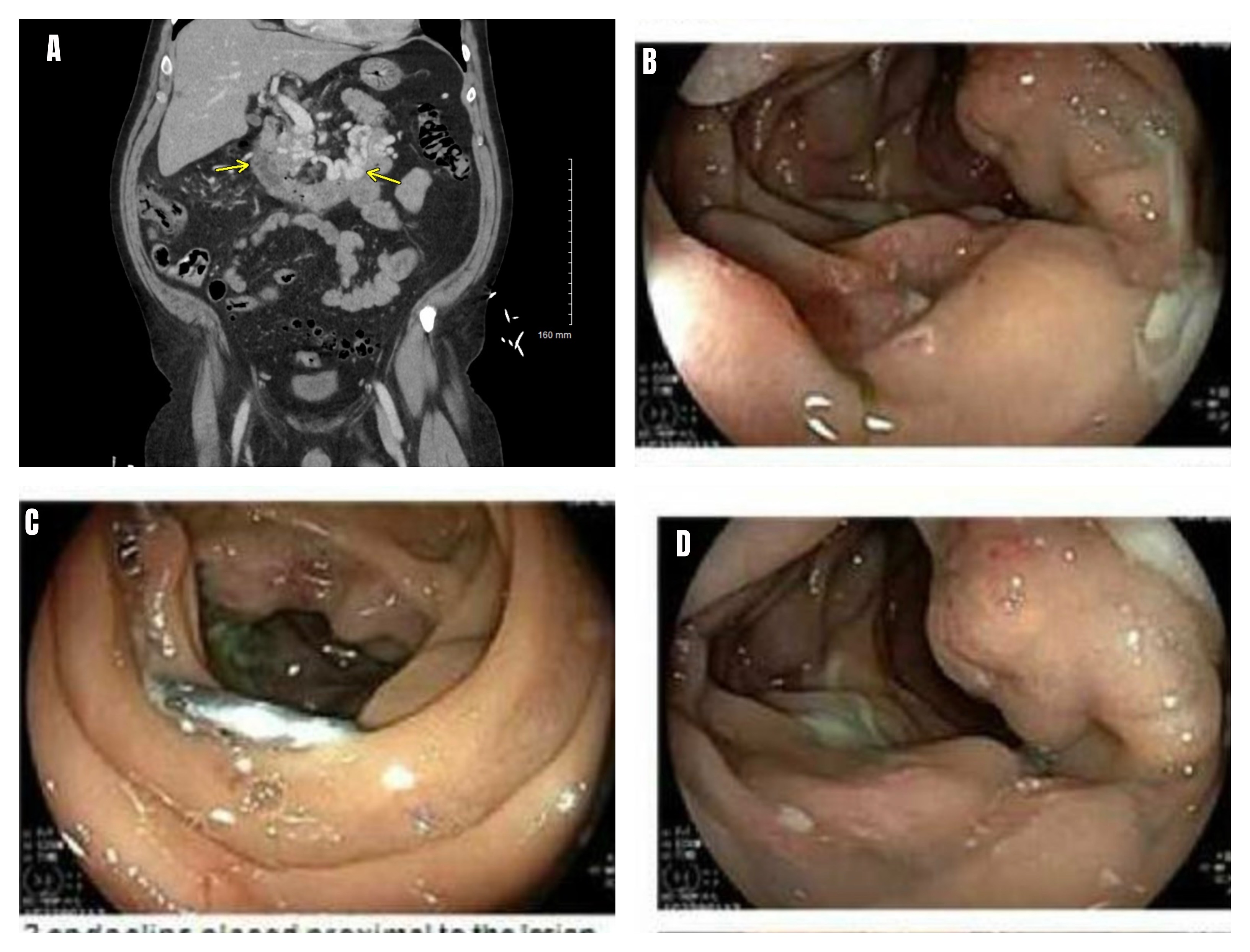
Figure: A. CT Angio with arrow marks denoting multiple dilated vessels, jejunal wall thickening
B,D. Columns of bleeding varices in the jejunum.
C. Endoclip applied for localisation.
B,D. Columns of bleeding varices in the jejunum.
C. Endoclip applied for localisation.
Disclosures:
Jagadish Koyi indicated no relevant financial relationships.
Mir Zulqarnain indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Anand Venugopal indicated no relevant financial relationships.
Wendell Clarkston indicated no relevant financial relationships.
Jagadish Koyi, MD1, Mir Zulqarnain, DO2, Mohamed Ahmed, MD3, Anand Venugopal, MD, PhD4, Wendell Clarkston, MD5. P4227 - Bleeding in the Shadows: Isolated Jejunal Varices Treated with Push Enteroscopy Sclerotherapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

