Tuesday Poster Session
Category: GI Bleeding
P4229 - Complexities in Managing Hemorrhagic Radiation Enteritis: An Endoscopist's Perspective and Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ariana R. Tagliaferri, MD
Creighton University Medical Center
Phoenix, AZ
Presenting Author(s)
Ariana R. Tagliaferri, MD1, Silpa Choday, MD2, Danielle Tran, BS3, Indu Srinivasan, MD1
1Creighton University Medical Center, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ; 3Creighton University School of Medicine, Omaha, NE
Introduction: Radiation-induced toxicity in the GI system leads to damage and loss of superficial epithelial cells, resulting in deposition of inflammatory infiltrates in the lamina propria. Acutely this manifests as hematochezia, diarrhea, incontinence; chronically, it can present with malabsorption, necrosis and strictures. There is no consensus on the treatment of these conditions, particularly in the management of small bowel hemorrhage, which can occur at any stage. While most studies describe symptomatic management of malabsorption and structural damage caused by radiation, literature on the diagnosis and treatment of hemorrhagic radiation enteritis remains limited.
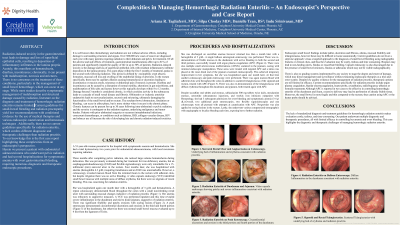
Case Description/Methods: A 53 year-old-woman with endometrial adenocarcinoma s/p total hysterectomy and local recurrence was seen for iron deficiency anemia (Hgb 3-4 g/dL) and hematochezia 3 months after completion of pelvic radiation. An initial EGD was normal, but a colonoscopy showed maroon blood from the terminal ileum to the rectum, but no active bleeding. A capsule endoscopy identified diffuse erythema of the small bowel without stigmata of bleeding. After recurrent transfusions, a repeat colonoscopy showed a rectal ulcer and radiation proctitis treated with APC. Despite sucralfate enemas and tablets following subsequent admissions, a capsule endoscopy diagnosed radiation enteritis in the distal duodenum and distal jejunum with significant friability and oozing. This was treated with APC during a subsequent push enteroscopy however the jejunal lesions could not be reached. A single balloon anterograde enteroscopy re-demonstrated radiation enteritis of the duodenum and jejunum with active bleeding treated with APC, however her hemoglobin was unresponsive to supportive measures. She ultimately had 5 subsequent admissions and underwent 2 flexible sigmoidoscopies, 3 push enteroscopies, 2 colonoscopies with APC cauterization and use of Nexpowder with minimal success.
Discussion: The lack of standardized diagnosis and treatment guidelines for hemorrhagic radiation enteritis makes evaluation costly, tedious, and time-consuming. Our patient underwent multiple diagnostic and therapeutic procedures, all with limited efficacy in controlling her anemia and overt bleeding. This case highlights the diagnostic and therapeutic challenges of managing hemorrhagic radiation enteritis.
Disclosures:
Ariana R. Tagliaferri, MD1, Silpa Choday, MD2, Danielle Tran, BS3, Indu Srinivasan, MD1. P4229 - Complexities in Managing Hemorrhagic Radiation Enteritis: An Endoscopist's Perspective and Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University Medical Center, Phoenix, AZ; 2Creighton University School of Medicine, Phoenix, AZ; 3Creighton University School of Medicine, Omaha, NE
Introduction: Radiation-induced toxicity in the GI system leads to damage and loss of superficial epithelial cells, resulting in deposition of inflammatory infiltrates in the lamina propria. Acutely this manifests as hematochezia, diarrhea, incontinence; chronically, it can present with malabsorption, necrosis and strictures. There is no consensus on the treatment of these conditions, particularly in the management of small bowel hemorrhage, which can occur at any stage. While most studies describe symptomatic management of malabsorption and structural damage caused by radiation, literature on the diagnosis and treatment of hemorrhagic radiation enteritis remains limited.
Case Description/Methods: A 53 year-old-woman with endometrial adenocarcinoma s/p total hysterectomy and local recurrence was seen for iron deficiency anemia (Hgb 3-4 g/dL) and hematochezia 3 months after completion of pelvic radiation. An initial EGD was normal, but a colonoscopy showed maroon blood from the terminal ileum to the rectum, but no active bleeding. A capsule endoscopy identified diffuse erythema of the small bowel without stigmata of bleeding. After recurrent transfusions, a repeat colonoscopy showed a rectal ulcer and radiation proctitis treated with APC. Despite sucralfate enemas and tablets following subsequent admissions, a capsule endoscopy diagnosed radiation enteritis in the distal duodenum and distal jejunum with significant friability and oozing. This was treated with APC during a subsequent push enteroscopy however the jejunal lesions could not be reached. A single balloon anterograde enteroscopy re-demonstrated radiation enteritis of the duodenum and jejunum with active bleeding treated with APC, however her hemoglobin was unresponsive to supportive measures. She ultimately had 5 subsequent admissions and underwent 2 flexible sigmoidoscopies, 3 push enteroscopies, 2 colonoscopies with APC cauterization and use of Nexpowder with minimal success.
Discussion: The lack of standardized diagnosis and treatment guidelines for hemorrhagic radiation enteritis makes evaluation costly, tedious, and time-consuming. Our patient underwent multiple diagnostic and therapeutic procedures, all with limited efficacy in controlling her anemia and overt bleeding. This case highlights the diagnostic and therapeutic challenges of managing hemorrhagic radiation enteritis.
Disclosures:
Ariana Tagliaferri indicated no relevant financial relationships.
Silpa Choday indicated no relevant financial relationships.
Danielle Tran indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Ariana R. Tagliaferri, MD1, Silpa Choday, MD2, Danielle Tran, BS3, Indu Srinivasan, MD1. P4229 - Complexities in Managing Hemorrhagic Radiation Enteritis: An Endoscopist's Perspective and Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
