Tuesday Poster Session
Category: GI Bleeding
P4230 - The GIST of an Upper GI Bleed
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- FL
Fredella Lee, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Fredella Lee, MD1, Michelle Lee, MD2, Ariel Bar-Mashiah, MD2, David Wan, MD1, Adnan Khdair, MD1, Tibor Krisko, MD1, Rasa Zarnegar, MD1
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction: Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors found in the GI tract, but are rare - constituting less than 3% of all GI malignancies. GISTs frequently present in the stomach (60%) and small bowel (20-30%), typically diagnosed in individuals greater than 50 years old. We report a case of an ulcerated proximal jejunal GIST in a young male who presented with upper GI bleeding.
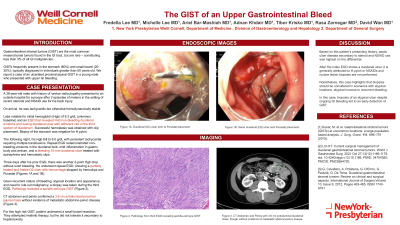
Case Description/Methods: A 38-year-old male with history of lumbar radiculopathy presented to an outside hospital for syncope after 2 episodes of melena in the setting of recent steroids and NSAID use for his back injury. On arrival, he was tachycardic but otherwise hemodynamically stable. Labs were notable for an initial hemoglobin (Hgb) of 6.3 g/dL (unknown baseline), and an EGD revealed mild non-bleeding duodenal erosions and oozing duodenal ulcer with adherent clot in the third section of duodenum. Successful hemostasis was obtained with clip placement. Biopsy of the stomach was negative for H. pylori. The following night, his Hgb fell to 6.0 g/dL with persistent tachycardia requiring multiple transfusions. Repeat EGD redemonstrated non-bleeding erosions in the duodenal bulb, mild inflammation in gastric body and antrum, and a bleeding 15-mm duodenal ulcer treated with epinephrine and hemostatic clips. Three days after his prior EGD, there was another 2-point Hgb drop without overt bleeding. He underwent repeat EGD showing a partially healed and friable D2 ulcer with hemorrhage stopped by hemoclips and Purastat. Given the recurrent nature of bleeding, atypical location and appearance, and need to rule out malignancy, a biopsy was taken during repeat EGD. Pathology revealed a spindle-cell type GIST. CT abdomen confirmed a 3.6 cm extraluminal proximal jejunal mass without evidence of metastatic abdomino-pelvic disease. For his high risk GIST, he underwent small bowel resection and did not tolerate imatinib therapy due to hepatotoxicity.
Discussion: With this patient’s history, peptic ulcer disease secondary to steroid and NSAID use was highest on the differential. After the index EGD shows a duodenal ulcer, it is generally attributed to H. pylori or NSAIDs and routine lesion biopsies are not performed. Nonetheless, this case highlights that biopsies should be considered in scenarios with atypical locations, atypical mucosa, or recurrent bleeding. In this case, biopsies of an atypical ulcer despite ongoing GI bleeding led to early detection of a GIST.

Disclosures:
Fredella Lee, MD1, Michelle Lee, MD2, Ariel Bar-Mashiah, MD2, David Wan, MD1, Adnan Khdair, MD1, Tibor Krisko, MD1, Rasa Zarnegar, MD1. P4230 - The GIST of an Upper GI Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, NY
Introduction: Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors found in the GI tract, but are rare - constituting less than 3% of all GI malignancies. GISTs frequently present in the stomach (60%) and small bowel (20-30%), typically diagnosed in individuals greater than 50 years old. We report a case of an ulcerated proximal jejunal GIST in a young male who presented with upper GI bleeding.
Case Description/Methods: A 38-year-old male with history of lumbar radiculopathy presented to an outside hospital for syncope after 2 episodes of melena in the setting of recent steroids and NSAID use for his back injury. On arrival, he was tachycardic but otherwise hemodynamically stable. Labs were notable for an initial hemoglobin (Hgb) of 6.3 g/dL (unknown baseline), and an EGD revealed mild non-bleeding duodenal erosions and oozing duodenal ulcer with adherent clot in the third section of duodenum. Successful hemostasis was obtained with clip placement. Biopsy of the stomach was negative for H. pylori. The following night, his Hgb fell to 6.0 g/dL with persistent tachycardia requiring multiple transfusions. Repeat EGD redemonstrated non-bleeding erosions in the duodenal bulb, mild inflammation in gastric body and antrum, and a bleeding 15-mm duodenal ulcer treated with epinephrine and hemostatic clips. Three days after his prior EGD, there was another 2-point Hgb drop without overt bleeding. He underwent repeat EGD showing a partially healed and friable D2 ulcer with hemorrhage stopped by hemoclips and Purastat. Given the recurrent nature of bleeding, atypical location and appearance, and need to rule out malignancy, a biopsy was taken during repeat EGD. Pathology revealed a spindle-cell type GIST. CT abdomen confirmed a 3.6 cm extraluminal proximal jejunal mass without evidence of metastatic abdomino-pelvic disease. For his high risk GIST, he underwent small bowel resection and did not tolerate imatinib therapy due to hepatotoxicity.
Discussion: With this patient’s history, peptic ulcer disease secondary to steroid and NSAID use was highest on the differential. After the index EGD shows a duodenal ulcer, it is generally attributed to H. pylori or NSAIDs and routine lesion biopsies are not performed. Nonetheless, this case highlights that biopsies should be considered in scenarios with atypical locations, atypical mucosa, or recurrent bleeding. In this case, biopsies of an atypical ulcer despite ongoing GI bleeding led to early detection of a GIST.

Figure: Figure A demonstrates a duodenal ulcer prior to PuraStat placement. Figure B demonstrates the same duodenal ulcer post PuraStat placement. Figure C demonstrates the 3.6cm extraluminal proximal jejunal mass on CT abdomen, detected after a positive biopsy.
Disclosures:
Fredella Lee indicated no relevant financial relationships.
Michelle Lee indicated no relevant financial relationships.
Ariel Bar-Mashiah indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Adnan Khdair indicated no relevant financial relationships.
Tibor Krisko indicated no relevant financial relationships.
Rasa Zarnegar indicated no relevant financial relationships.
Fredella Lee, MD1, Michelle Lee, MD2, Ariel Bar-Mashiah, MD2, David Wan, MD1, Adnan Khdair, MD1, Tibor Krisko, MD1, Rasa Zarnegar, MD1. P4230 - The GIST of an Upper GI Bleed, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
