Tuesday Poster Session
Category: General Endoscopy
P4149 - Transhepatic Percutaneous Gastrostomy Tube Placement: Complications and Considerations Prior to Endoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- IN
Induja R. Nimma, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Induja R. Nimma, MD1, Brittany S. Jackson, MD1, Rex Siu, MD1, Ryan J. Hoffman, DO2, Jana G. Hashash, MD, MSc1
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Interventional Radiology, Jacksonville, FL
Introduction: We present a case of a percutaneous gastrostomy tube (PGT) inadvertently inserted through the liver. This case was complicated by hematemesis with consideration of endoscopic evaluation (EGD). We highlight the potential consequences of transhepatic PGT placement and risks to consider before performing EGD.
Case Description/Methods: A 22-year-old male with a history of renal transplant, encapsulated peritoneal sclerosis from peritoneal dialysis, small bowel obstruction (SBO), and deep vein thrombosis (on heparin), presented with abdominal pain, distension (APD), and SBO.
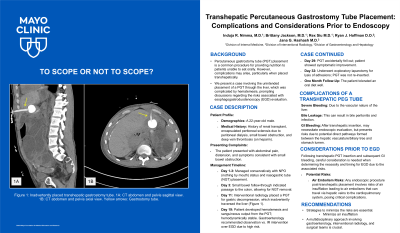
The patient was managed conservatively with NPO status and nasogastric tube (NGT) placement. On day 3, small bowel follow-through showed contrast at the colon in 4.3 hours, allowing NGT removal. However, the patient experienced worsening APD and emesis with persistent SBO on X-ray, requiring NGT re-insertion. On day 11, interventional radiology (IR) placed a PGT for gastric decompression, which inadvertently traversed the liver (Figure 1). This led to an abdominal wall hematoma requiring blood transfusion and exacerbated APD.
On day 19, the patient had hematemesis and sanguineous output from the PGT. As the patient was hemodynamically stable, gastroenterology recommended observation vs IR intervention over EGD due to the high procedural risk and low probability for endoscopic therapeutics as bleeding was likely from the liver. The patient’s hemoglobin stabilized, and bleeding resolved. The PGT accidently fell out on day 29, coinciding with symptomatic improvement. On day 32, exploratory laparotomy for lysis of adhesions with partial peritonectomy was performed and the PGT was not re-inserted. At one month follow-up, the patient tolerated an oral diet well.
Discussion: Transhepatic placement of a PGT can result in significant consequences due to the liver's vascular nature, leading to severe bleeding and bile leakage which may cause bile peritonitis and infection.
GI bleeding after transhepatic PGT insertion may warrant EGD, but the risk of creating a direct pathway between hepatic vasculature/biliary tree and the stomach lumen raises significant concerns. There is a risk of introducing an air embolism while using air insufflation needed for endoscopic visibility. Air embolisms can travel via hepatic veins to the cardiopulmonary system, causing critical complications. If an EGD is crucial, a multidisciplinary approach involving GI, IR, and surgery is recommended, employing strategies to minimize insufflation to mitigate risks.

Disclosures:
Induja R. Nimma, MD1, Brittany S. Jackson, MD1, Rex Siu, MD1, Ryan J. Hoffman, DO2, Jana G. Hashash, MD, MSc1. P4149 - Transhepatic Percutaneous Gastrostomy Tube Placement: Complications and Considerations Prior to Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Interventional Radiology, Jacksonville, FL
Introduction: We present a case of a percutaneous gastrostomy tube (PGT) inadvertently inserted through the liver. This case was complicated by hematemesis with consideration of endoscopic evaluation (EGD). We highlight the potential consequences of transhepatic PGT placement and risks to consider before performing EGD.
Case Description/Methods: A 22-year-old male with a history of renal transplant, encapsulated peritoneal sclerosis from peritoneal dialysis, small bowel obstruction (SBO), and deep vein thrombosis (on heparin), presented with abdominal pain, distension (APD), and SBO.
The patient was managed conservatively with NPO status and nasogastric tube (NGT) placement. On day 3, small bowel follow-through showed contrast at the colon in 4.3 hours, allowing NGT removal. However, the patient experienced worsening APD and emesis with persistent SBO on X-ray, requiring NGT re-insertion. On day 11, interventional radiology (IR) placed a PGT for gastric decompression, which inadvertently traversed the liver (Figure 1). This led to an abdominal wall hematoma requiring blood transfusion and exacerbated APD.
On day 19, the patient had hematemesis and sanguineous output from the PGT. As the patient was hemodynamically stable, gastroenterology recommended observation vs IR intervention over EGD due to the high procedural risk and low probability for endoscopic therapeutics as bleeding was likely from the liver. The patient’s hemoglobin stabilized, and bleeding resolved. The PGT accidently fell out on day 29, coinciding with symptomatic improvement. On day 32, exploratory laparotomy for lysis of adhesions with partial peritonectomy was performed and the PGT was not re-inserted. At one month follow-up, the patient tolerated an oral diet well.
Discussion: Transhepatic placement of a PGT can result in significant consequences due to the liver's vascular nature, leading to severe bleeding and bile leakage which may cause bile peritonitis and infection.
GI bleeding after transhepatic PGT insertion may warrant EGD, but the risk of creating a direct pathway between hepatic vasculature/biliary tree and the stomach lumen raises significant concerns. There is a risk of introducing an air embolism while using air insufflation needed for endoscopic visibility. Air embolisms can travel via hepatic veins to the cardiopulmonary system, causing critical complications. If an EGD is crucial, a multidisciplinary approach involving GI, IR, and surgery is recommended, employing strategies to minimize insufflation to mitigate risks.

Figure: Figure 1: Inadvertently placed transhepatic gastrostomy tube. 1A: CT abdomen and pelvis sagittal view. 1B: CT abdomen and pelvis axial view. Yellow arrows: Gastrostomy tube.
Disclosures:
Induja Nimma indicated no relevant financial relationships.
Brittany Jackson indicated no relevant financial relationships.
Rex Siu indicated no relevant financial relationships.
Ryan Hoffman indicated no relevant financial relationships.
Jana Hashash: Bristol Myers Squibb – Consultant.
Induja R. Nimma, MD1, Brittany S. Jackson, MD1, Rex Siu, MD1, Ryan J. Hoffman, DO2, Jana G. Hashash, MD, MSc1. P4149 - Transhepatic Percutaneous Gastrostomy Tube Placement: Complications and Considerations Prior to Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
