Tuesday Poster Session
Category: General Endoscopy
P4151 - Amyloidosis: A Rare Cause of Pan-Dysmotility
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RJ
Rofina Johnkennedy, MD, MPH
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Rofina Johnkennedy, MD1, Cheng-Hung Tai, MD1, Alexa Plato, MD1, Xi Wang, MD, PhD2, Michelle Hughes, MD3
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale New Haven Health, New Haven, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Amyloidosis is a rare systemic infiltrative disease, with a prevalence estimated to be 6-10 cases per million person-years. It involves the extracellular deposition of beta-sheet fibrillar protein and can manifest in any organ system in the body. Diagnosis of gastrointestinal involvement of amyloidosis can be difficult, given its nonspecific symptoms including abdominal pain, nausea, dysphagia, and diarrhea. We present a rare case of AL amyloidosis with pan-gastrointestinal involvement.
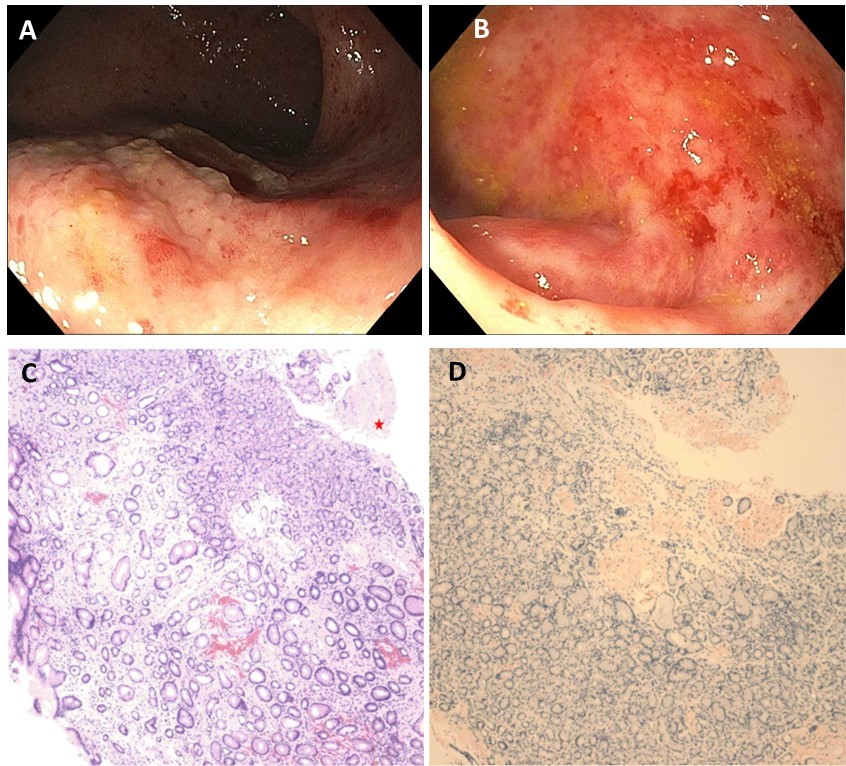
Case Description/Methods: A 56 year old female with paroxysmal atrial fibrillation, pre-diabetes, obesity, IBS, and bilateral carpal tunnel syndrome presented with fatigue, dysphagia, and constipation. Standard lab testing was unremarkable. The patient underwent EGD and sigmoidoscopy with biopsies obtained from the esophagus, stomach, duodenum, and rectosigmoid colon. Endoscopic visualization showed nodular and erythematous gastric antrum, pale duodenum with hypervascular mucosa, and friable rectal mucosa with loss of vascularity. Pathology showed amyloid deposits in the proximal and distal esophagus, stomach, duodenum, and rectosigmoid colon. Samples sent to Mayo Clinic confirmed AL lambda-type amyloid. Four months after discharge, the patient had worsening dysphagia and gastroparesis, requiring PEG-J tube placement. She is undergoing systemic therapy with daratumumab, cyclophosphamide, bortezomib, and dexamethasone.
Discussion: Gastrointestinal amyloidosis poses significant diagnostic and treatment challenges. Patients present with nonspecific symptoms and diagnosis relies on pathological evaluation of tissue samples showing green birefringence on Congo red staining. This patient’s predominant and nonspecific gastrointestinal manifestations raised concern for amyloidosis due to her history of progressive dysphagia, early satiety, and constipation. In one prospective cohort study, diffuse amyloid deposition of the GI tract is rare (1%), and carries an overall median survival of 8 months. Heightened awareness may lead to earlier detection, with improvement in overall survival and quality-adjusted life years.
Disclosures:
Rofina Johnkennedy, MD1, Cheng-Hung Tai, MD1, Alexa Plato, MD1, Xi Wang, MD, PhD2, Michelle Hughes, MD3. P4151 - Amyloidosis: A Rare Cause of Pan-Dysmotility, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2Yale New Haven Health, New Haven, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Amyloidosis is a rare systemic infiltrative disease, with a prevalence estimated to be 6-10 cases per million person-years. It involves the extracellular deposition of beta-sheet fibrillar protein and can manifest in any organ system in the body. Diagnosis of gastrointestinal involvement of amyloidosis can be difficult, given its nonspecific symptoms including abdominal pain, nausea, dysphagia, and diarrhea. We present a rare case of AL amyloidosis with pan-gastrointestinal involvement.
Case Description/Methods: A 56 year old female with paroxysmal atrial fibrillation, pre-diabetes, obesity, IBS, and bilateral carpal tunnel syndrome presented with fatigue, dysphagia, and constipation. Standard lab testing was unremarkable. The patient underwent EGD and sigmoidoscopy with biopsies obtained from the esophagus, stomach, duodenum, and rectosigmoid colon. Endoscopic visualization showed nodular and erythematous gastric antrum, pale duodenum with hypervascular mucosa, and friable rectal mucosa with loss of vascularity. Pathology showed amyloid deposits in the proximal and distal esophagus, stomach, duodenum, and rectosigmoid colon. Samples sent to Mayo Clinic confirmed AL lambda-type amyloid. Four months after discharge, the patient had worsening dysphagia and gastroparesis, requiring PEG-J tube placement. She is undergoing systemic therapy with daratumumab, cyclophosphamide, bortezomib, and dexamethasone.
Discussion: Gastrointestinal amyloidosis poses significant diagnostic and treatment challenges. Patients present with nonspecific symptoms and diagnosis relies on pathological evaluation of tissue samples showing green birefringence on Congo red staining. This patient’s predominant and nonspecific gastrointestinal manifestations raised concern for amyloidosis due to her history of progressive dysphagia, early satiety, and constipation. In one prospective cohort study, diffuse amyloid deposition of the GI tract is rare (1%), and carries an overall median survival of 8 months. Heightened awareness may lead to earlier detection, with improvement in overall survival and quality-adjusted life years.
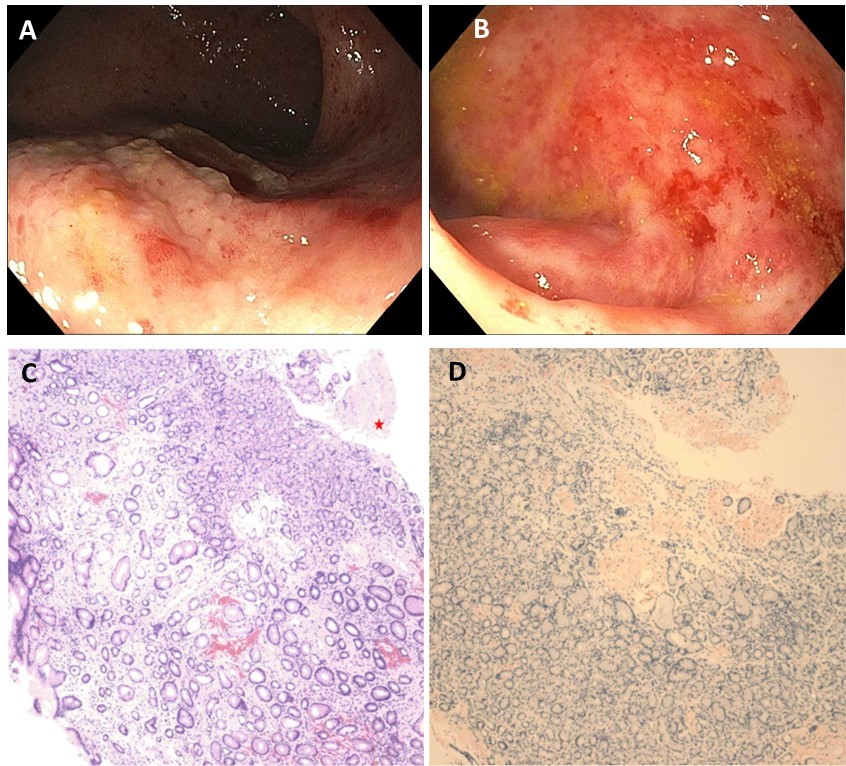
Figure: A. Gastric body on endoscopic visualization.
B. Rectum on endoscopic visualization.
C. H&E stain of the stomach biopsy shows deposition of pink amorphous material (red asterisk).
D. Congo red stain highlights diffuse infiltration of the amyloid materials.
B. Rectum on endoscopic visualization.
C. H&E stain of the stomach biopsy shows deposition of pink amorphous material (red asterisk).
D. Congo red stain highlights diffuse infiltration of the amyloid materials.
Disclosures:
Rofina Johnkennedy indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Alexa Plato indicated no relevant financial relationships.
Xi Wang indicated no relevant financial relationships.
Michelle Hughes: Iterative Health – Consultant. PureVu – Consultant.
Rofina Johnkennedy, MD1, Cheng-Hung Tai, MD1, Alexa Plato, MD1, Xi Wang, MD, PhD2, Michelle Hughes, MD3. P4151 - Amyloidosis: A Rare Cause of Pan-Dysmotility, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
