Tuesday Poster Session
Category: Functional Bowel Disease
P4066 - Association Between Rosacea and Gastrointestinal Disorders: A Single-Center Retrospective Cohort Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ER
Elizabeth Reznik, MD
New York-Presbyterian/Weill Cornell
New York, NY
Presenting Author(s)
Elizabeth Reznik, MD
New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Rosacea is a prevalent chronic inflammatory disease that primarily affects the central face and is characterized by flushing, persistent erythema, telangiectasia, and inflammatory papules and pustules. Among various comorbidities, rosacea has been commonly associated with gastrointestinal disorders such as inflammatory bowel disease, Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and <em>Helicobacter pylori</em> infection, although prior studies have demonstrated equivocal results. This relationship may in part be mediated by the gut microbiome and its role in the inflammatory cutaneous response.
Methods: This is a single-center retrospective cohort study using TriNetX, a global federated research network providing statistics on electronic health records. The analytics subset contained data from approximately 2.6 million patients in the Weill Cornell Health Care Organization. The records of patients between the ages of 18 and 75 with rosacea were identified based on ICD-10 codes, as well as co-occurring diagnoses of inflammatory bowel disease (Crohn’s disease and ulcerative colitis), Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and <em>H. pylori</em> infection.
Results: Of nearly 2.6 million patients included in this study, 15,110 patients carried a diagnosis of rosacea based on ICD-10 coding. 72.5% of patients diagnosed with rosacea were female, and 59.2% were white. Table 1 demonstrates the demographic data of patients with or without rosacea (control) and whether patients were also diagnosed with inflammatory bowel disease, Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and <em>H. pylori infection</em>. When stratified by sex, female patients with rosacea were statistically significantly more likely to be diagnosed with all aforementioned gastrointestinal disorders (p < 0.0001).
Discussion: This study indicates that patients with rosacea are associated with an increase in prevalence of gastrointestinal disorders. While the mechanism underlying this association is unclear, these findings suggest that there appears to be a correlation between rosacea and various gastrointestinal comorbidities, highlighting the possibility that aberrations in the gut-skin axis may be implicated in the pathogenesis of rosacea. Greater understanding of this condition and the effects of the gut-skin axis can allow for more timely and efficacious treatment.
Disclosures:
Elizabeth Reznik, MD. P4066 - Association Between Rosacea and Gastrointestinal Disorders: A Single-Center Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Rosacea is a prevalent chronic inflammatory disease that primarily affects the central face and is characterized by flushing, persistent erythema, telangiectasia, and inflammatory papules and pustules. Among various comorbidities, rosacea has been commonly associated with gastrointestinal disorders such as inflammatory bowel disease, Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and <em>Helicobacter pylori</em> infection, although prior studies have demonstrated equivocal results. This relationship may in part be mediated by the gut microbiome and its role in the inflammatory cutaneous response.
Methods: This is a single-center retrospective cohort study using TriNetX, a global federated research network providing statistics on electronic health records. The analytics subset contained data from approximately 2.6 million patients in the Weill Cornell Health Care Organization. The records of patients between the ages of 18 and 75 with rosacea were identified based on ICD-10 codes, as well as co-occurring diagnoses of inflammatory bowel disease (Crohn’s disease and ulcerative colitis), Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and <em>H. pylori</em> infection.
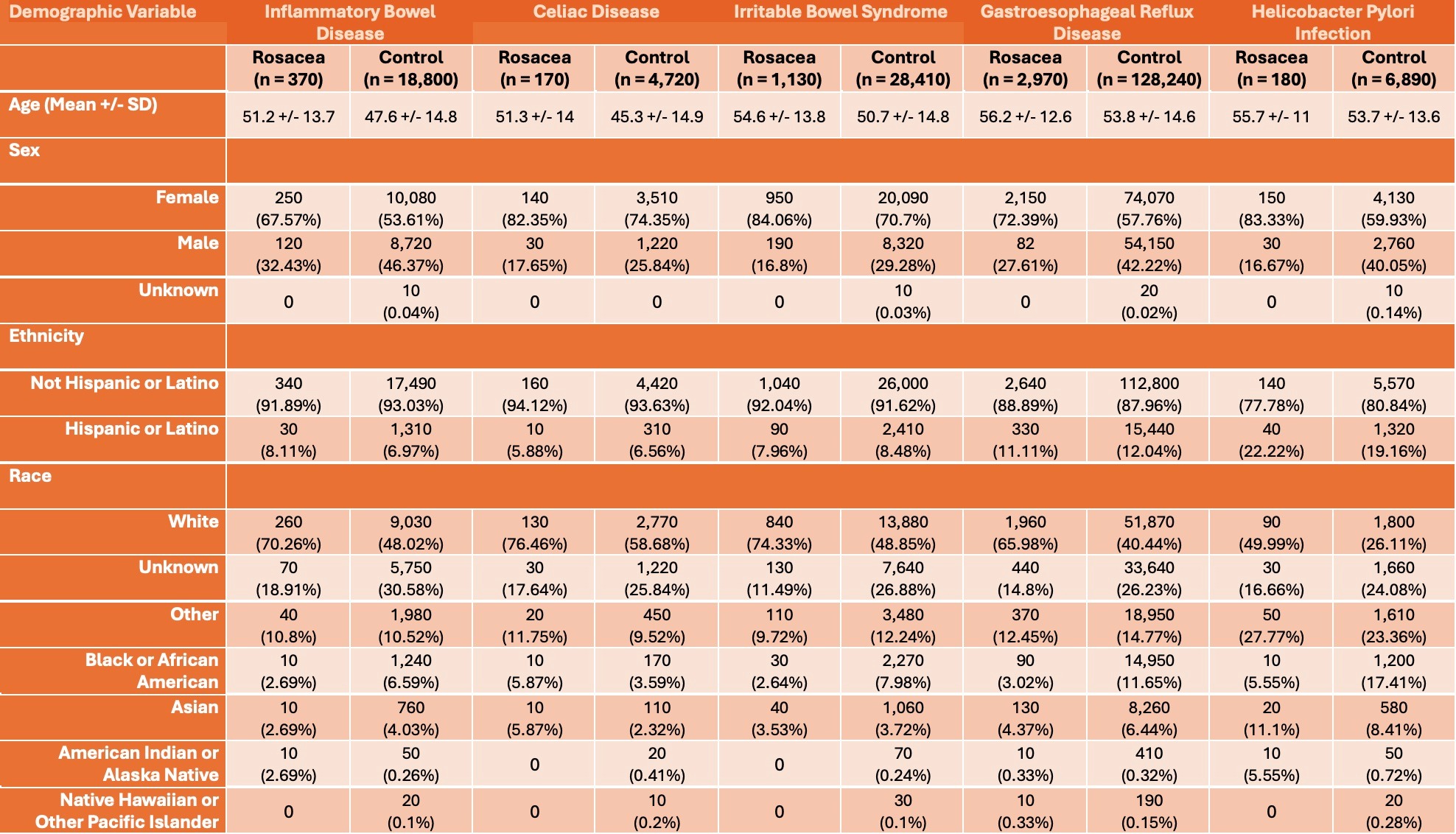
Results: Of nearly 2.6 million patients included in this study, 15,110 patients carried a diagnosis of rosacea based on ICD-10 coding. 72.5% of patients diagnosed with rosacea were female, and 59.2% were white. Table 1 demonstrates the demographic data of patients with or without rosacea (control) and whether patients were also diagnosed with inflammatory bowel disease, Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and <em>H. pylori infection</em>. When stratified by sex, female patients with rosacea were statistically significantly more likely to be diagnosed with all aforementioned gastrointestinal disorders (p < 0.0001).
Discussion: This study indicates that patients with rosacea are associated with an increase in prevalence of gastrointestinal disorders. While the mechanism underlying this association is unclear, these findings suggest that there appears to be a correlation between rosacea and various gastrointestinal comorbidities, highlighting the possibility that aberrations in the gut-skin axis may be implicated in the pathogenesis of rosacea. Greater understanding of this condition and the effects of the gut-skin axis can allow for more timely and efficacious treatment.
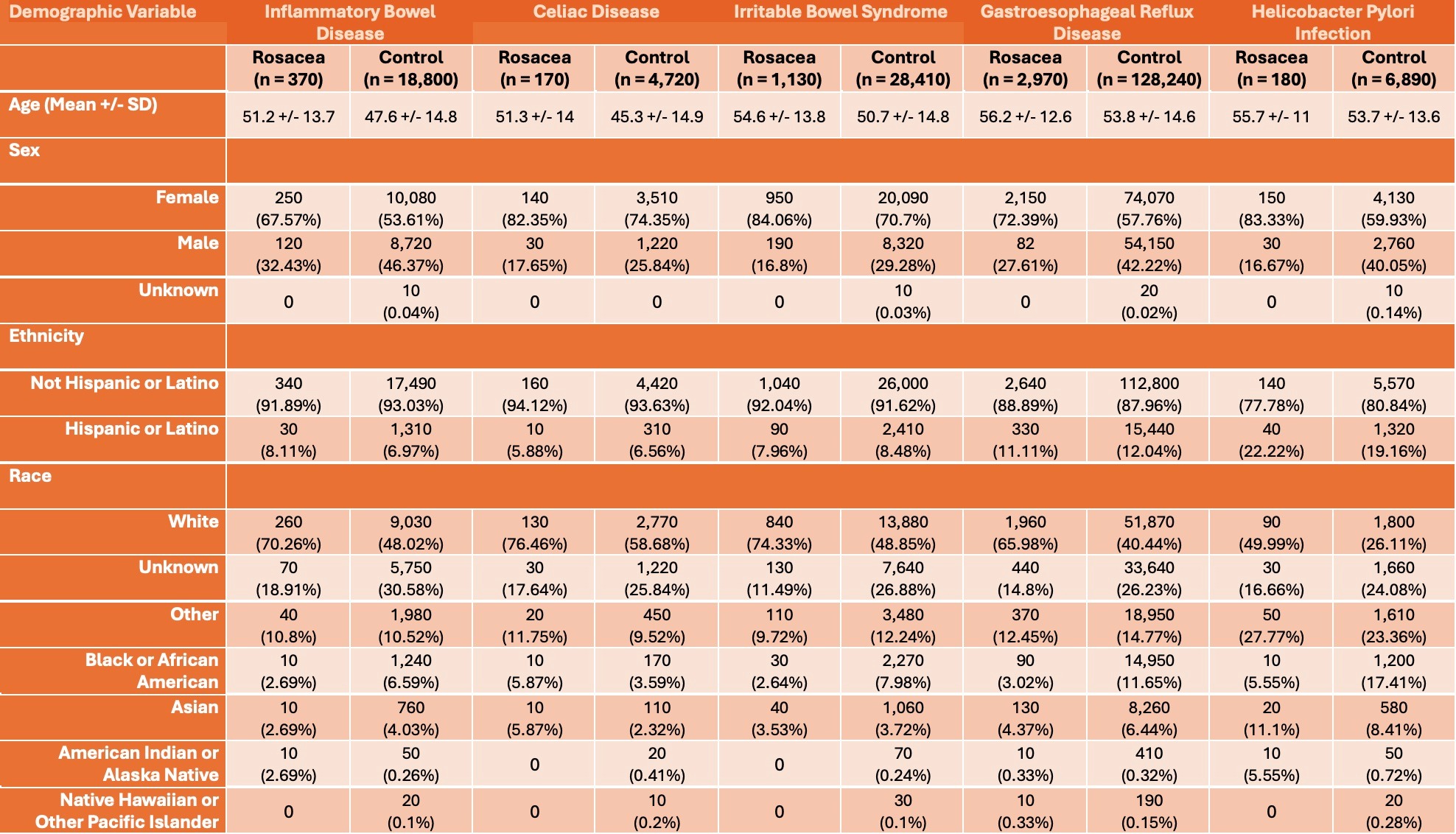
Figure: Table 1. Demographic variables including age (mean +/- standard deviation), sex, ethnicity, and race. Patients with inflammatory bowel disease, Celiac disease, irritable bowel syndrome, gastroesophageal reflux disease, and Helicobacter Pylori Infection were stratified based on whether patients were diagnosed with Rosacea or not (Control).
Disclosures:
Elizabeth Reznik indicated no relevant financial relationships.
Elizabeth Reznik, MD. P4066 - Association Between Rosacea and Gastrointestinal Disorders: A Single-Center Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
