Tuesday Poster Session
Category: Esophagus
P3989 - Esophageal Squamous Cell Carcinoma Presenting as a Tracheoesophageal Fistula: Clinical Insights From a Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nida Ansari, DO
St. Joseph's University Medical Center
Flanders, NJ
Presenting Author(s)
Nida Ansari, DO1, Karam Zakharia, MD2, Noor Bittar, BS2, Gabriel Melki, MD2, Yana Cavanagh, MD2
1St. Joseph's University Medical Center, Flanders, NJ; 2St. Joseph's University Medical Center, Paterson, NJ
Introduction: Esophageal cancer (EC) is the 11th leading cause of cancer-related deaths in the US, with a 5-year survival rate of 21.7%. The presentation of EC include weight loss, bleeding, throat pain, hoarseness, and dysphagia, which is more pronounced when the esophageal lumen is narrowed to one-third of its normal diameter. Squamous cell carcinoma (SCC) affects the proximal to mid-esophagus and adenocarcinoma typically presents in the distal esophagus. In proximal EC, increasing cough can indicate tracheoesophageal fistula (TEF). TEF can be seen as a complication of treatment or in end-stage disease.
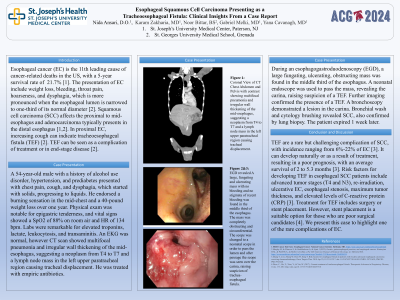
Case Description/Methods: A 54-year-old male with a history of alcohol use disorder, hypertension, and prediabetes presented with chest pain, cough, and dysphagia, which started with solids, progressing to liquids. He endorsed a burning sensation in the mid-chest and a 40-pound weight loss over one year. Physical exam was notable for epigastric tenderness, and vital signs showed a SpO2 of 88% on room air and HR of 134 bpm. Labs were remarkable for elevated troponins, lactate, leukocytosis, and transaminitis. An EKG was normal, however CT scan showed multifocal pneumonia and irregular wall thickening of the mid-esophagus, suggesting a neoplasm from T4 to T7 and a lymph node mass in the left upper paratracheal region causing tracheal displacement. He was treated with empiric antibiotics.
During an esophagogastroduodenoscopy (EGD), a large fungating, ulcerating, obstructing mass was found in the middle third of the esophagus. A neonatal endoscope was used to pass the mass, revealing the carina, raising suspicion of a TEF. Further imaging confirmed the presence of a TEF. A bronchoscopy demonstrated a lesion in the carina. Bronchial wash and cytology brushing revealed SCC, also confirmed by lung biopsy. The patient expired 1 week later.
Discussion: TEF are a rare but challenging complication of SCC, with incidence ranging from 6%-22% of EC. It can develop naturally or as a result of treatment, resulting in a poor prognosis, with an average survival of 2 to 5.3 months. Risk factors for developing TEF in esophageal SCC patients include advanced tumor stages (T4 and N3), re-irradiation, ulcerative EC, esophageal stenosis, maximum tumor thickness, and elevated levels of C-reactive protein (CRP). Treatment for TEF includes surgery or stent placement. However, stent placement is a suitable option for those who are poor poor surgical candidates. We present this case to highlight one of the rare complications of EC.
Disclosures:
Nida Ansari, DO1, Karam Zakharia, MD2, Noor Bittar, BS2, Gabriel Melki, MD2, Yana Cavanagh, MD2. P3989 - Esophageal Squamous Cell Carcinoma Presenting as a Tracheoesophageal Fistula: Clinical Insights From a Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Joseph's University Medical Center, Flanders, NJ; 2St. Joseph's University Medical Center, Paterson, NJ
Introduction: Esophageal cancer (EC) is the 11th leading cause of cancer-related deaths in the US, with a 5-year survival rate of 21.7%. The presentation of EC include weight loss, bleeding, throat pain, hoarseness, and dysphagia, which is more pronounced when the esophageal lumen is narrowed to one-third of its normal diameter. Squamous cell carcinoma (SCC) affects the proximal to mid-esophagus and adenocarcinoma typically presents in the distal esophagus. In proximal EC, increasing cough can indicate tracheoesophageal fistula (TEF). TEF can be seen as a complication of treatment or in end-stage disease.
Case Description/Methods: A 54-year-old male with a history of alcohol use disorder, hypertension, and prediabetes presented with chest pain, cough, and dysphagia, which started with solids, progressing to liquids. He endorsed a burning sensation in the mid-chest and a 40-pound weight loss over one year. Physical exam was notable for epigastric tenderness, and vital signs showed a SpO2 of 88% on room air and HR of 134 bpm. Labs were remarkable for elevated troponins, lactate, leukocytosis, and transaminitis. An EKG was normal, however CT scan showed multifocal pneumonia and irregular wall thickening of the mid-esophagus, suggesting a neoplasm from T4 to T7 and a lymph node mass in the left upper paratracheal region causing tracheal displacement. He was treated with empiric antibiotics.
During an esophagogastroduodenoscopy (EGD), a large fungating, ulcerating, obstructing mass was found in the middle third of the esophagus. A neonatal endoscope was used to pass the mass, revealing the carina, raising suspicion of a TEF. Further imaging confirmed the presence of a TEF. A bronchoscopy demonstrated a lesion in the carina. Bronchial wash and cytology brushing revealed SCC, also confirmed by lung biopsy. The patient expired 1 week later.
Discussion: TEF are a rare but challenging complication of SCC, with incidence ranging from 6%-22% of EC. It can develop naturally or as a result of treatment, resulting in a poor prognosis, with an average survival of 2 to 5.3 months. Risk factors for developing TEF in esophageal SCC patients include advanced tumor stages (T4 and N3), re-irradiation, ulcerative EC, esophageal stenosis, maximum tumor thickness, and elevated levels of C-reactive protein (CRP). Treatment for TEF includes surgery or stent placement. However, stent placement is a suitable option for those who are poor poor surgical candidates. We present this case to highlight one of the rare complications of EC.
Disclosures:
Nida Ansari indicated no relevant financial relationships.
Karam Zakharia indicated no relevant financial relationships.
Noor Bittar indicated no relevant financial relationships.
Gabriel Melki indicated no relevant financial relationships.
Yana Cavanagh indicated no relevant financial relationships.
Nida Ansari, DO1, Karam Zakharia, MD2, Noor Bittar, BS2, Gabriel Melki, MD2, Yana Cavanagh, MD2. P3989 - Esophageal Squamous Cell Carcinoma Presenting as a Tracheoesophageal Fistula: Clinical Insights From a Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
