Tuesday Poster Session
Category: Esophagus
P3991 - Like Daughter, Like Mother: A Familial Case of Achalasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Mahmoud Mahdi, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Mahmoud Mahdi, MD1, Micah Vander Griend, MPH1, Marisa-Nicole Zayat, MD1, Diala Merheb, MD1, Estephan Zayat, MD2
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
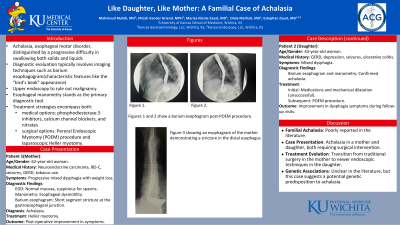
Introduction: Achalasia, a rare esophageal motor disorder, is distinguished by a progressive difficulty in swallowing both solids and liquids. Diagnostic evaluation typically involves imaging techniques such as barium esophagogram to reveal characteristic features like the "bird's beak" appearance and absence of peristalsis, along with upper endoscopy to rule out malignancy. Esophageal manometry stands as the primary diagnostic tool. Treatment strategies encompass both medical options, like phosphodiesterase-5 inhibitors, calcium channel blockers, and nitrates, as well as surgical interventions, such as the Peroral Endoscopic Myotomy (POEM) procedure and laparoscopic Heller myotomy.
Case Description/Methods: A 62-year-old woman with a past medical history of neuroendocrine carcinoma, IBS-C, seizures, GERD, and tobacco use presented to our clinic reporting progressive mixed dysphagia with weight loss. EGD revealed normal mucosa but was suspicious for spasms. Manometry revealed esophageal dysmotility, followed by a barium esophagram indicating a short segment stricture of the distal esophagus at the gastroesophageal junction, confirming a diagnosis of achalasia. A shared decision was made to proceed with a Heller myotomy. The patient’s symptoms improved post-operatively.
Intriguingly, ten years later, her biological daughter, a 43-year-old woman with a medical history notable for GERD, depression, seizures, and ulcerative colitis, also presented to our clinic complaining of mixed dysphagia. Barium esophagram and manometry studies confirmed a diagnosis of achalasia. Following unsuccessful resolution of symptoms with medications and mechanical dilatation, she underwent a POEM procedure. In subsequent follow-up visits, the patient experienced improvement in her dysphagia symptoms.
Discussion: Familial cases of achalasia are poorly reported in the literature. Here, we present a case of familial achalasia in a mother and her daughter, both necessitating surgical intervention for symptom management. It is also interesting how the “surgical” approach changed from mother to daughter with the introduction of newer endoscopic techniques. Although genetic associations with dysphagia remain unclear in the literature, cases like the one presented herein highlight the prospect of genetic predisposition underlying this condition.
Disclosures:
Mahmoud Mahdi, MD1, Micah Vander Griend, MPH1, Marisa-Nicole Zayat, MD1, Diala Merheb, MD1, Estephan Zayat, MD2. P3991 - Like Daughter, Like Mother: A Familial Case of Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Achalasia, a rare esophageal motor disorder, is distinguished by a progressive difficulty in swallowing both solids and liquids. Diagnostic evaluation typically involves imaging techniques such as barium esophagogram to reveal characteristic features like the "bird's beak" appearance and absence of peristalsis, along with upper endoscopy to rule out malignancy. Esophageal manometry stands as the primary diagnostic tool. Treatment strategies encompass both medical options, like phosphodiesterase-5 inhibitors, calcium channel blockers, and nitrates, as well as surgical interventions, such as the Peroral Endoscopic Myotomy (POEM) procedure and laparoscopic Heller myotomy.
Case Description/Methods: A 62-year-old woman with a past medical history of neuroendocrine carcinoma, IBS-C, seizures, GERD, and tobacco use presented to our clinic reporting progressive mixed dysphagia with weight loss. EGD revealed normal mucosa but was suspicious for spasms. Manometry revealed esophageal dysmotility, followed by a barium esophagram indicating a short segment stricture of the distal esophagus at the gastroesophageal junction, confirming a diagnosis of achalasia. A shared decision was made to proceed with a Heller myotomy. The patient’s symptoms improved post-operatively.
Intriguingly, ten years later, her biological daughter, a 43-year-old woman with a medical history notable for GERD, depression, seizures, and ulcerative colitis, also presented to our clinic complaining of mixed dysphagia. Barium esophagram and manometry studies confirmed a diagnosis of achalasia. Following unsuccessful resolution of symptoms with medications and mechanical dilatation, she underwent a POEM procedure. In subsequent follow-up visits, the patient experienced improvement in her dysphagia symptoms.
Discussion: Familial cases of achalasia are poorly reported in the literature. Here, we present a case of familial achalasia in a mother and her daughter, both necessitating surgical intervention for symptom management. It is also interesting how the “surgical” approach changed from mother to daughter with the introduction of newer endoscopic techniques. Although genetic associations with dysphagia remain unclear in the literature, cases like the one presented herein highlight the prospect of genetic predisposition underlying this condition.
Disclosures:
Mahmoud Mahdi indicated no relevant financial relationships.
Micah Vander Griend indicated no relevant financial relationships.
Marisa-Nicole Zayat indicated no relevant financial relationships.
Diala Merheb indicated no relevant financial relationships.
Estephan Zayat indicated no relevant financial relationships.
Mahmoud Mahdi, MD1, Micah Vander Griend, MPH1, Marisa-Nicole Zayat, MD1, Diala Merheb, MD1, Estephan Zayat, MD2. P3991 - Like Daughter, Like Mother: A Familial Case of Achalasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
