Tuesday Poster Session
Category: Esophagus
P3993 - The Role of Endoscopy in Aortoenteric Fistula Diagnosis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KD
Kathryn Driggers, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Kathryn Driggers, MD1, Kyler Kozacek, DO2, John G.. McCarthy, MD1
1Walter Reed National Military Medical Center, Bethesda, MD; 2William Beaumont Hospital, El Paso, TX
Introduction: Aortoenteric fistulas (AEF) are a feared but rare complication of endovascular surgery, with mortality rates approaching 50%. Endoscopic approaches to temporize bleeding have been described, however definitive repair is surgical. We present a case of an endoscopically confirmed aortoenteric fistula after a herald bleed in a man with an extensive endovascular history.
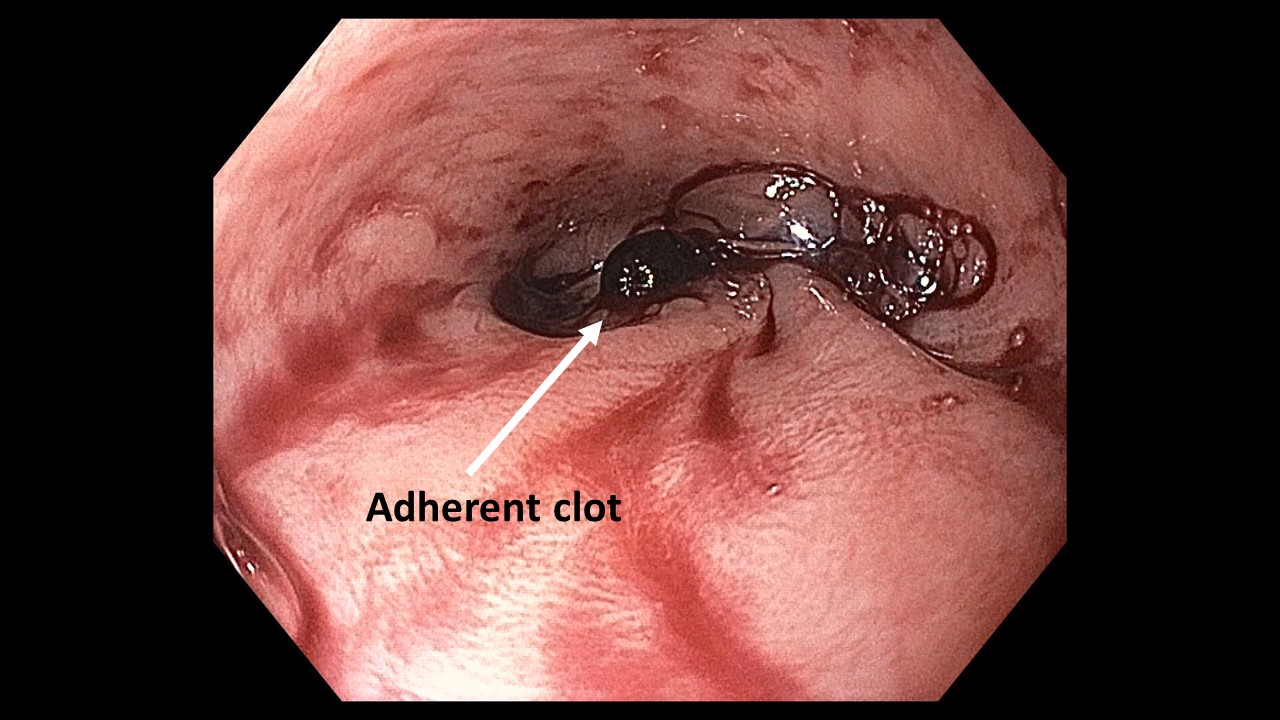
Case Description/Methods: A 68-year-old man with a thoracic endovascular aortic repair (TEVAR) and aorto-celiac bypass presented to the emergency room for hematemesis. His prior TEVAR had been complicated by esophageal injury intraoperatively and esophageal rupture days later. The rupture was successfully repaired via fully covered esophageal stent but then was complicated by aortic graft infection prompting subtotal graft explant and lifelong IV antibiotics. On this presentation, a CT scan demonstrated graft infection progression and a possible aorto-esophageal fistula. During a prior GI bleed, there had also been radiographic concern for AEF, however, he had no endoscopic evidence of an AEF then. Given his surgical history, an AEF was difficult to confirm radiographically, and surgical options were highly morbid. In concert with family and vascular surgery support, we performed an EGD to evaluate. This demonstrated an adherent pulsating clot at the distal esophagus consistent with an AEF. The EGD was aborted, and the patient was brought back to the intensive care unit for ongoing family discussion and care per the vascular surgery team. He unfortunately expired a few hours later due to exsanguinating hemorrhage.
Discussion: AEFs are a rare but highly morbid cause of GI bleeding which can exist in either the thoracic or abdominal aorta. Secondary AEFs are more common than primary and are most commonly due to prior endovascular surgery with graft placement. Definitive management of AEFs is endovascular repair. Endoscopy may serve an adjunctive role in temporizing active bleeding (stenting, endoscopic balloon inflation, Hemospray), repair of luminal esophageal defects after endovascular repair (clips, stenting), and as in this case, in clarifying diagnostic uncertainty. Endoscopy has been reported to have a low sensitivity (25% in one 2005 review) for non-bleeding AEFs, however CT, which is the standard first line imaging choice, is only 61% sensitive. In cases such as this one, where prior surgical and infectious history makes CT interpretation challenging, endoscopic assessment can serve as an important adjunct in AEF diagnosis.
Disclosures:
Kathryn Driggers, MD1, Kyler Kozacek, DO2, John G.. McCarthy, MD1. P3993 - The Role of Endoscopy in Aortoenteric Fistula Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Walter Reed National Military Medical Center, Bethesda, MD; 2William Beaumont Hospital, El Paso, TX
Introduction: Aortoenteric fistulas (AEF) are a feared but rare complication of endovascular surgery, with mortality rates approaching 50%. Endoscopic approaches to temporize bleeding have been described, however definitive repair is surgical. We present a case of an endoscopically confirmed aortoenteric fistula after a herald bleed in a man with an extensive endovascular history.
Case Description/Methods: A 68-year-old man with a thoracic endovascular aortic repair (TEVAR) and aorto-celiac bypass presented to the emergency room for hematemesis. His prior TEVAR had been complicated by esophageal injury intraoperatively and esophageal rupture days later. The rupture was successfully repaired via fully covered esophageal stent but then was complicated by aortic graft infection prompting subtotal graft explant and lifelong IV antibiotics. On this presentation, a CT scan demonstrated graft infection progression and a possible aorto-esophageal fistula. During a prior GI bleed, there had also been radiographic concern for AEF, however, he had no endoscopic evidence of an AEF then. Given his surgical history, an AEF was difficult to confirm radiographically, and surgical options were highly morbid. In concert with family and vascular surgery support, we performed an EGD to evaluate. This demonstrated an adherent pulsating clot at the distal esophagus consistent with an AEF. The EGD was aborted, and the patient was brought back to the intensive care unit for ongoing family discussion and care per the vascular surgery team. He unfortunately expired a few hours later due to exsanguinating hemorrhage.
Discussion: AEFs are a rare but highly morbid cause of GI bleeding which can exist in either the thoracic or abdominal aorta. Secondary AEFs are more common than primary and are most commonly due to prior endovascular surgery with graft placement. Definitive management of AEFs is endovascular repair. Endoscopy may serve an adjunctive role in temporizing active bleeding (stenting, endoscopic balloon inflation, Hemospray), repair of luminal esophageal defects after endovascular repair (clips, stenting), and as in this case, in clarifying diagnostic uncertainty. Endoscopy has been reported to have a low sensitivity (25% in one 2005 review) for non-bleeding AEFs, however CT, which is the standard first line imaging choice, is only 61% sensitive. In cases such as this one, where prior surgical and infectious history makes CT interpretation challenging, endoscopic assessment can serve as an important adjunct in AEF diagnosis.
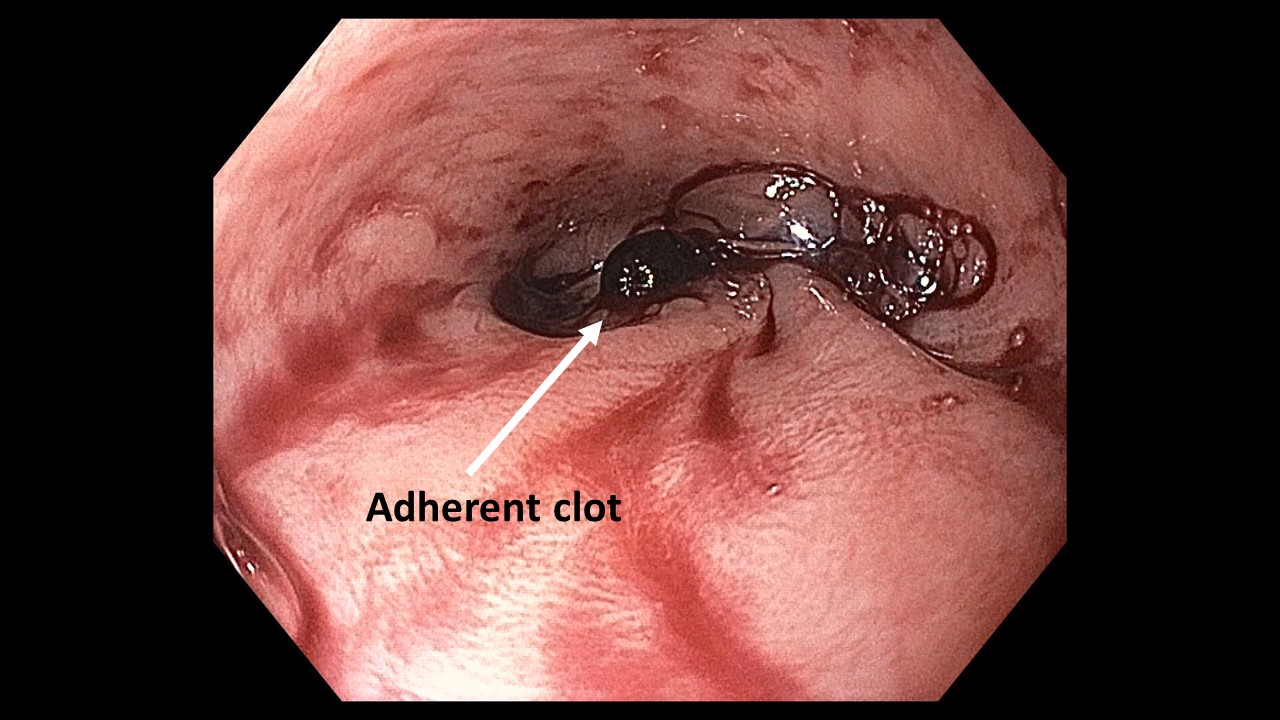
Figure: Distal esophagus with adherent pulsating clot
Disclosures:
Kathryn Driggers indicated no relevant financial relationships.
Kyler Kozacek indicated no relevant financial relationships.
John McCarthy indicated no relevant financial relationships.
Kathryn Driggers, MD1, Kyler Kozacek, DO2, John G.. McCarthy, MD1. P3993 - The Role of Endoscopy in Aortoenteric Fistula Diagnosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
