Monday Poster Session
Category: Liver
P2919 - The ABCs of PBC: Alkaline Phosphatase, Biliary Health, and Candidacy for Obeticholic Acid Treatment
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JW
Jordan Woodard, MD
University of Kentucky College of Medicine
Lexington, KY
Presenting Author(s)
Jordan Woodard, MD1, Mary Hunter Hyche, BS2, Austin Bambach, DO3, Andre Eaddy, MD, PhD3
1University of Kentucky College of Medicine, Lexington, KY; 2Prisma Health, University of South Carolina School of Medicine, Greenville, SC; 3Prisma Health Greenville Memorial Hospital, Greenville, SC
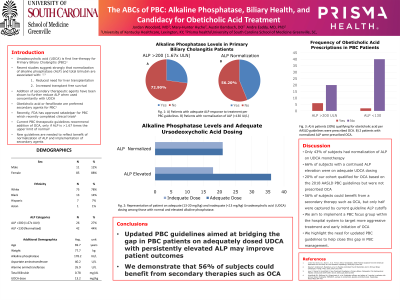
Introduction: Ursodeoxycholic acid (UDCA) is first line-therapy for Primary Biliary Cholangitis (PBC). Recent studies suggest strongly that normalization of alkaline phosphatase (ALP) and total bilirubin are associated with reduced need for liver transplantation and increased transplant free survival. Addition of a secondary therapeutic agent such as Obeticholic acid (OCA) have been shown to further reduce ALP when used concomitantly with UDCA. Current PBC therapeutic guidelines recommend addition of OCA, only if ALP is >1.67 times the upper limit of normal, which suggests a gap in care to PBC patients who would benefit from normalization of ALP.
Methods: We performed a retrospective analysis of 107 PBC patients on UDCA therapy at a tertiary care center. Inclusion criteria included age >18 years, current UDCA prescription for at least 12 months, and liver enzymes within the past 12 months. General demographics, liver enzymes and weight-based UDCA dose was calculated based on most recent prescription. An ALP of 200 IU/L was determined 1.67 times the upper limit normal for and normalization of ALP was 130 IU/L or lower. An adequate daily UDCA dose was at least 13 mg/kg daily. Statistical analysis was completed via Microsoft Excel.
Results: A total of 96 subjects were included in the study. Subjects were 89% were female and 78% were white. Average ALP and total bilirubin were 178 IU/L and 0.8 mg/dL, respectively. Almost 60% of the cohort was prescribed 13 mg/kg UDCA or higher dose. ALP >200 IU/L was present in 26 subjects (27%) but only 6 were prescribed OCA. An ALP elevation >130 IU/L was present in 54 subjects (56%), and, of these, 33% were on < 13mg/kg of UDCA.
Discussion: Only 43% of subjects had normalization of ALP on UDCA monotherapy. Sixty-six percent of subjects with a continued ALP elevation were on adequate UDCA dosing. Twenty percent of our cohort qualified for OCA based on the 2018 AASLD PBC guidelines but were not prescribed OCA. With known improvement in outcomes such as transplant-free survival in those with normalized ALP and bilirubin, we demonstrate that 56% of subjects could benefit from a secondary therapy such as OCA. We aim to implement a PBC focus group within the hospital system to target more aggressive treatment and early initiation of OCA. We highlight the need for updated PBC guidelines to help close this gap in PBC management.
Disclosures:
Jordan Woodard, MD1, Mary Hunter Hyche, BS2, Austin Bambach, DO3, Andre Eaddy, MD, PhD3. P2919 - The ABCs of PBC: Alkaline Phosphatase, Biliary Health, and Candidacy for Obeticholic Acid Treatment, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kentucky College of Medicine, Lexington, KY; 2Prisma Health, University of South Carolina School of Medicine, Greenville, SC; 3Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Ursodeoxycholic acid (UDCA) is first line-therapy for Primary Biliary Cholangitis (PBC). Recent studies suggest strongly that normalization of alkaline phosphatase (ALP) and total bilirubin are associated with reduced need for liver transplantation and increased transplant free survival. Addition of a secondary therapeutic agent such as Obeticholic acid (OCA) have been shown to further reduce ALP when used concomitantly with UDCA. Current PBC therapeutic guidelines recommend addition of OCA, only if ALP is >1.67 times the upper limit of normal, which suggests a gap in care to PBC patients who would benefit from normalization of ALP.
Methods: We performed a retrospective analysis of 107 PBC patients on UDCA therapy at a tertiary care center. Inclusion criteria included age >18 years, current UDCA prescription for at least 12 months, and liver enzymes within the past 12 months. General demographics, liver enzymes and weight-based UDCA dose was calculated based on most recent prescription. An ALP of 200 IU/L was determined 1.67 times the upper limit normal for and normalization of ALP was 130 IU/L or lower. An adequate daily UDCA dose was at least 13 mg/kg daily. Statistical analysis was completed via Microsoft Excel.
Results: A total of 96 subjects were included in the study. Subjects were 89% were female and 78% were white. Average ALP and total bilirubin were 178 IU/L and 0.8 mg/dL, respectively. Almost 60% of the cohort was prescribed 13 mg/kg UDCA or higher dose. ALP >200 IU/L was present in 26 subjects (27%) but only 6 were prescribed OCA. An ALP elevation >130 IU/L was present in 54 subjects (56%), and, of these, 33% were on < 13mg/kg of UDCA.
Discussion: Only 43% of subjects had normalization of ALP on UDCA monotherapy. Sixty-six percent of subjects with a continued ALP elevation were on adequate UDCA dosing. Twenty percent of our cohort qualified for OCA based on the 2018 AASLD PBC guidelines but were not prescribed OCA. With known improvement in outcomes such as transplant-free survival in those with normalized ALP and bilirubin, we demonstrate that 56% of subjects could benefit from a secondary therapy such as OCA. We aim to implement a PBC focus group within the hospital system to target more aggressive treatment and early initiation of OCA. We highlight the need for updated PBC guidelines to help close this gap in PBC management.
Disclosures:
Jordan Woodard indicated no relevant financial relationships.
Mary Hunter Hyche indicated no relevant financial relationships.
Austin Bambach indicated no relevant financial relationships.
Andre Eaddy: Abbvie – Speakers Bureau.
Jordan Woodard, MD1, Mary Hunter Hyche, BS2, Austin Bambach, DO3, Andre Eaddy, MD, PhD3. P2919 - The ABCs of PBC: Alkaline Phosphatase, Biliary Health, and Candidacy for Obeticholic Acid Treatment, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
