Monday Poster Session
Category: Liver
P2929 - Metabolic Risk Factors and Ursodiol Response in Primary Biliary Cholangitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Spyridon Zouridis, MD
SSM Health Saint Louis University Hospital
St. Louis, MO
Presenting Author(s)
Spyridon Zouridis, MD1, Khang Nguyen, 2, Felicia Lee, MD2, Kamran Qureshi, MD2
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2Saint Louis University School of Medicine, St. Louis, MO
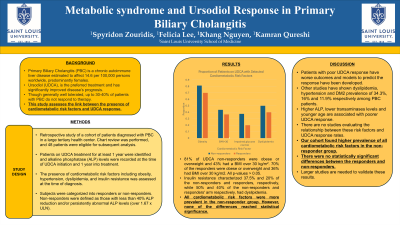
Introduction: Primary Biliary Cholangitis (PBC) is a chronic autoimmune liver disease estimated to affect 14.6 per 100,000 persons worldwide, predominantly females. Ursodiol (UDCA), is the preferred treatment and has significantly improved disease’s prognosis. Even though it is generally well tolerated, up to 30-40% of patients with PBC do not respond to therapy. This study assesses the link between the presence of cardiometabolic risk factors and UDCA response.
Methods: A cohort of 214 patients diagnosed with PBC in a large tertiary health center was retrospectively studied. Patients with overlap syndrome and other chronic liver disease except Metabolic Dysfunction Associated Liver Disease (MASLD) were excluded. The presence of cardiometabolic risk factors including obesity, hypertension, hyperlipidemia, and insulin resistance was assessed at the time of diagnosis. Patients on UDCA treatment for at least 1 year were identified and alkaline phosphatase (ALP) levels were recorded at the time of UDCA initiation and 1 year into treatment. 48 patients were eligible for subsequent analysis. Subjects were categorized into responders or non-responders. Non-responders were defined as those with less than 40% ALP reduction and/or persistently abnormal ALP levels (over 1.67 x ULN).
Results: Upon analysis, 81% of UDCA non-responders were obese, and 43% had a BMI over 30 kg/m2. On the other hand, 70% of the responders were obese and 36% had BMI over 30 kg/m2. Insulin resistance characterized 37.5% and 20% of the non-responders and responders respectively. 50% and 40% of the non-responders and responders arm respectively, had dyslipidemia. All cardiometabolic risk factors were more prevalent in the non-responder group. However, none of the differences reached statistical significance.
Discussion: Other studies show hyperlipidemia, hypertension and DM2 prevalence of 34.3%, 16% and 11.9% respectively among PBC patients. Patients with poor UDCA response have worse outcomes and models to predict the response have been developed. Higher ALP, lower transaminases levels and younger age are associated with poorer UDCA response. There is no adequate data on the relationship between metabolic risk factors and UDCA response rates. In our cohort we found higher prevalence of all cardiometabolic risk factors in the non-responder group. However, there were no statistically significant differences between the responders and non-responders. Larger studies are needed to validate these results.
Disclosures:
Spyridon Zouridis, MD1, Khang Nguyen, 2, Felicia Lee, MD2, Kamran Qureshi, MD2. P2929 - Metabolic Risk Factors and Ursodiol Response in Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2Saint Louis University School of Medicine, St. Louis, MO
Introduction: Primary Biliary Cholangitis (PBC) is a chronic autoimmune liver disease estimated to affect 14.6 per 100,000 persons worldwide, predominantly females. Ursodiol (UDCA), is the preferred treatment and has significantly improved disease’s prognosis. Even though it is generally well tolerated, up to 30-40% of patients with PBC do not respond to therapy. This study assesses the link between the presence of cardiometabolic risk factors and UDCA response.
Methods: A cohort of 214 patients diagnosed with PBC in a large tertiary health center was retrospectively studied. Patients with overlap syndrome and other chronic liver disease except Metabolic Dysfunction Associated Liver Disease (MASLD) were excluded. The presence of cardiometabolic risk factors including obesity, hypertension, hyperlipidemia, and insulin resistance was assessed at the time of diagnosis. Patients on UDCA treatment for at least 1 year were identified and alkaline phosphatase (ALP) levels were recorded at the time of UDCA initiation and 1 year into treatment. 48 patients were eligible for subsequent analysis. Subjects were categorized into responders or non-responders. Non-responders were defined as those with less than 40% ALP reduction and/or persistently abnormal ALP levels (over 1.67 x ULN).
Results: Upon analysis, 81% of UDCA non-responders were obese, and 43% had a BMI over 30 kg/m2. On the other hand, 70% of the responders were obese and 36% had BMI over 30 kg/m2. Insulin resistance characterized 37.5% and 20% of the non-responders and responders respectively. 50% and 40% of the non-responders and responders arm respectively, had dyslipidemia. All cardiometabolic risk factors were more prevalent in the non-responder group. However, none of the differences reached statistical significance.
Discussion: Other studies show hyperlipidemia, hypertension and DM2 prevalence of 34.3%, 16% and 11.9% respectively among PBC patients. Patients with poor UDCA response have worse outcomes and models to predict the response have been developed. Higher ALP, lower transaminases levels and younger age are associated with poorer UDCA response. There is no adequate data on the relationship between metabolic risk factors and UDCA response rates. In our cohort we found higher prevalence of all cardiometabolic risk factors in the non-responder group. However, there were no statistically significant differences between the responders and non-responders. Larger studies are needed to validate these results.
Disclosures:
Spyridon Zouridis indicated no relevant financial relationships.
Khang Nguyen indicated no relevant financial relationships.
Felicia Lee indicated no relevant financial relationships.
Kamran Qureshi: Intercept Pharmaceuticals – Speakers Bureau. Madrigal Pharmaceuticals – Speakers Bureau. Phathom Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Spyridon Zouridis, MD1, Khang Nguyen, 2, Felicia Lee, MD2, Kamran Qureshi, MD2. P2929 - Metabolic Risk Factors and Ursodiol Response in Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
