Monday Poster Session
Category: Liver
P2933 - Evaluating Differences in Screening Between Pediatric and Adult Patients for Development of Metabolic Dysfunction-Associated Steatotic Liver Disease at an Academic Primary Care Clinic
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harris Feldman, MD
UMass Chan Medical School
Worcester, MA
Presenting Author(s)
Harris Feldman, MD1, Xiang Li, MS1, Kayla Wilson, MD1, Suzanne Sprague, MD1, Deepika Devuni, MD2
1UMass Chan Medical School, Worcester, MA; 2University of Massachusetts Memorial Medical Center, Worcester, MA
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most common liver disease in both pediatric and adult populations with a rising prevalence of 7.40% and 32.4%, respectively. Current literature suggests MASLD will be the leading cause of liver transplantation in young adults over the next decade. Presently, guidelines recommend screening children with metabolic risk factors using alanine aminotransferase (ALT), while adult populations should be screened with blood testing and abdominal imaging. It is critical to better understand current screening practices for MASLD in pediatric as compared to adult populations to reduce future morbidity and mortality.
Methods: We conducted a single-center, retrospective, cohort study of patients with diagnosis codes associated with increased risk for developing MASLD, seen at a combined internal medicine-pediatrics clinic that cares for approximately 50% children and 50% adults. Included diagnosis codes correlated to being overweight or obese (32 codes), having prediabetes or type-2 diabetes (3 codes), having elevated cholesterol (9 codes), or having pre-hypertension or essential hypertension (9 codes). Patients were stratified into a pediatric group, aged 10 to 22 years old, and an adult group, aged greater than 23 years old. Incidence of liver enzyme testing, abdominal imaging, associated diagnoses with MASLD, and referrals to nutrition were measured.
Results: 89 pediatric-aged patients and 1115 adult-aged patients met our study criteria, and a higher incidence of comorbidities were seen in the adult-aged group (p< 0.05). Similar rates of liver function blood testing were performed in both groups (47% and 53%, p=0.05); however, for liver imaging, there were 0 incidences in the pediatric group compared to 5% of the adult group (p=0.24). A sub-analysis of the pediatric group (n=89) stratified by age 10-17 and 18-22 showed similar rates of screening with liver function testing (50% vs. 41%, p=0.20). For referrals, a higher percentage of nutritional referrals were placed for the pediatric group compared to the adult group (68% vs. 12%) (p=0.17).
Discussion: This study demonstrates that screening rates for MASLD using blood testing for liver function were approximately equal across children and adults; however, screening using abdominal imaging is not as prevalent in this clinic. Future initiatives are needed to evaluate the impact of using abdominal imaging for MASLD screening in children.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harris Feldman, MD1, Xiang Li, MS1, Kayla Wilson, MD1, Suzanne Sprague, MD1, Deepika Devuni, MD2. P2933 - Evaluating Differences in Screening Between Pediatric and Adult Patients for Development of Metabolic Dysfunction-Associated Steatotic Liver Disease at an Academic Primary Care Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1UMass Chan Medical School, Worcester, MA; 2University of Massachusetts Memorial Medical Center, Worcester, MA
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most common liver disease in both pediatric and adult populations with a rising prevalence of 7.40% and 32.4%, respectively. Current literature suggests MASLD will be the leading cause of liver transplantation in young adults over the next decade. Presently, guidelines recommend screening children with metabolic risk factors using alanine aminotransferase (ALT), while adult populations should be screened with blood testing and abdominal imaging. It is critical to better understand current screening practices for MASLD in pediatric as compared to adult populations to reduce future morbidity and mortality.
Methods: We conducted a single-center, retrospective, cohort study of patients with diagnosis codes associated with increased risk for developing MASLD, seen at a combined internal medicine-pediatrics clinic that cares for approximately 50% children and 50% adults. Included diagnosis codes correlated to being overweight or obese (32 codes), having prediabetes or type-2 diabetes (3 codes), having elevated cholesterol (9 codes), or having pre-hypertension or essential hypertension (9 codes). Patients were stratified into a pediatric group, aged 10 to 22 years old, and an adult group, aged greater than 23 years old. Incidence of liver enzyme testing, abdominal imaging, associated diagnoses with MASLD, and referrals to nutrition were measured.
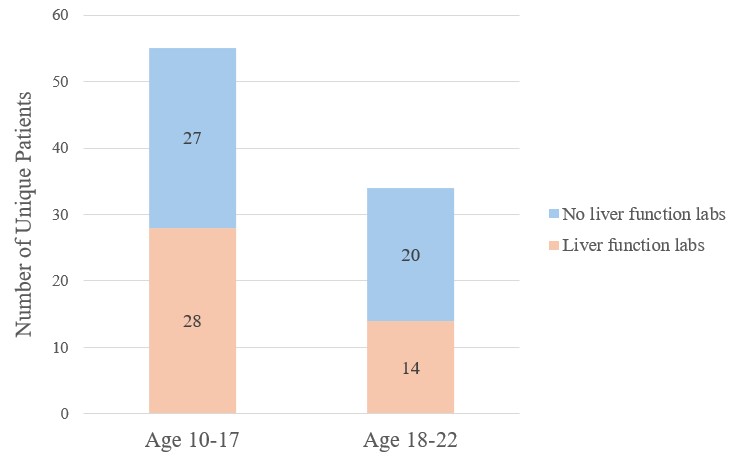
Results: 89 pediatric-aged patients and 1115 adult-aged patients met our study criteria, and a higher incidence of comorbidities were seen in the adult-aged group (p< 0.05). Similar rates of liver function blood testing were performed in both groups (47% and 53%, p=0.05); however, for liver imaging, there were 0 incidences in the pediatric group compared to 5% of the adult group (p=0.24). A sub-analysis of the pediatric group (n=89) stratified by age 10-17 and 18-22 showed similar rates of screening with liver function testing (50% vs. 41%, p=0.20). For referrals, a higher percentage of nutritional referrals were placed for the pediatric group compared to the adult group (68% vs. 12%) (p=0.17).
Discussion: This study demonstrates that screening rates for MASLD using blood testing for liver function were approximately equal across children and adults; however, screening using abdominal imaging is not as prevalent in this clinic. Future initiatives are needed to evaluate the impact of using abdominal imaging for MASLD screening in children.
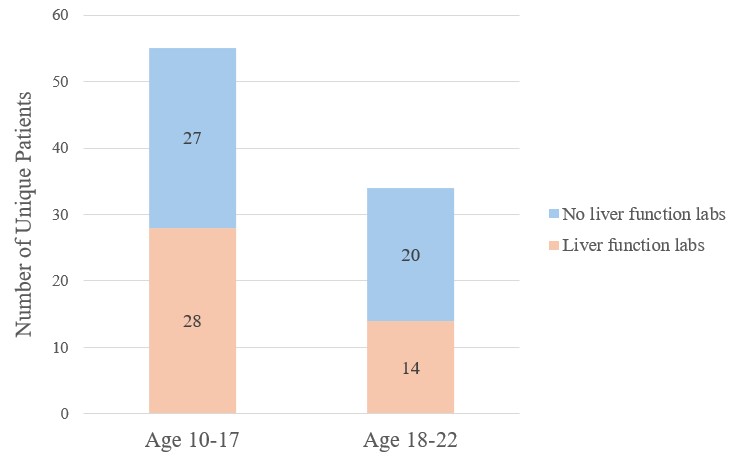
Figure: Figure 1. Sub-analysis of MASLD screening using liver function labs for the pediatric group stratified by age 10-17 and 18-22 (n=89). Similar rates of screening were found in both groups (50% vs. 41%, p=0.20)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Harris Feldman indicated no relevant financial relationships.
Xiang Li indicated no relevant financial relationships.
Kayla Wilson indicated no relevant financial relationships.
Suzanne Sprague indicated no relevant financial relationships.
Deepika Devuni: Massachusetts Department of Public Health – Grant/Research Support. National Institute on Alcohol Abuse and Alcoholism – Grant/Research Support. Sequana Medical – Grant/Research Support.
Harris Feldman, MD1, Xiang Li, MS1, Kayla Wilson, MD1, Suzanne Sprague, MD1, Deepika Devuni, MD2. P2933 - Evaluating Differences in Screening Between Pediatric and Adult Patients for Development of Metabolic Dysfunction-Associated Steatotic Liver Disease at an Academic Primary Care Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

