Monday Poster Session
Category: Liver
P2964 - Liver Disease Mortality in the United States: Demographic Shifts from 1999 to 2020
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nosheen Hafeez, MD
Baptist Health-University of Arkansas for Medical Sciences
North Little Rock, AR
Presenting Author(s)
Nosheen Hafeez, MD1, Ehab Alkhawaldeh, MD2, Sabri Elmansouri, MD, MPH3, Bachar Hamad, MD4, Sammy Hamad, DO5, Mohamed Boshnaf, MD, MPH6
1Baptist Health-University of Arkansas for Medical Sciences, North Little Rock, AR; 2Albalaq Applied University, Lockport, IL; 3Insight Hospital and Medical Center, Chicago, IL; 4Ascension Saint Joseph Hospital, Joliet, IL; 5Ascension Saint Joseph Medical Center, Joliet, IL; 6Baptist Health UAMS, North Little Rock, AR
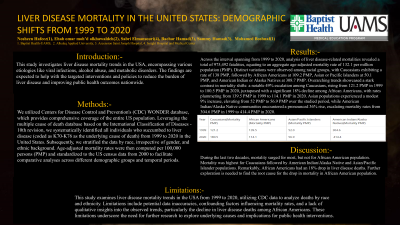
Introduction: This study investigates liver disease mortality trends in the USA, encompassing various etiologies like viral infections, alcohol abuse, and metabolic disorders. The findings are expected to help with the targeted interventions and policies to reduce the burden of liver disease and improving public health outcomes nationwide.
Methods: We ultilized Centers for Disease Control and Prevention's (CDC) WONDER database, which provides comprehensive coverage of the entire US population. Leveraging the multiple cause of death database based on the International Classification of Diseases - 10th revision, we systematically identified all individuals who succumbed to liver disease (coded as K70-K76 as the underlying cause of death) from 1999 to 2020 in the United States. Subsequently, we stratified the data by race, irrespective of gender, and ethnic background. Age-adjusted mortality rates were then computed per 100,000 persons (PMP) and standardized to the US census data from 2000 to facilitate comparative analyses across different demographic groups and temporal periods.
Results: Across the interval spanning from 1999 to 2020, analysis of liver disease-related mortalities revealed a total of 975,492 fatalities, equating to an aggregate age-adjusted mortality rate of 132.1 per million population (PMP). Distinct variations were observed among racial groups, with Caucasians exhibiting a rate of 138 PMP, followed by African Americans at 109.2 PMP, Asian or Pacific Islanders at 50.1 PMP, and American Indian or Alaska Natives at 308.7 PMP. Overarching trends showcased a stark contrast in mortality shifts: a notable 49% escalation among Caucasians, rising from 121.2 PMP in 1999 to 180.5 PMP in 2020, juxtaposed with a significant 18% decline among African Americans, with rates plummeting from 139.5 PMP in 1999 to 114.1 PMP in 2020. Asian populations experienced a modest 9% increase, elevating from 52 PMP to 56.9 PMP over the studied period, while American Indian/Alaska Native communities encountered a pronounced 36% rise, escalating mortality rates from 304.6 PMP in 1999 to 414.4 PMP in 2020.
Discussion: During the last two decades, mortality surged for most, but not for African American population. Mortality was highest for Caucasians followed by American Indian/Alaska Native and Asian/Pacific Islander populations. Remarkably, African Americans had an 18% drop in liver disease deaths. Further exploration is needed to find the root cause for the drop in mortality in African American population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nosheen Hafeez, MD1, Ehab Alkhawaldeh, MD2, Sabri Elmansouri, MD, MPH3, Bachar Hamad, MD4, Sammy Hamad, DO5, Mohamed Boshnaf, MD, MPH6. P2964 - Liver Disease Mortality in the United States: Demographic Shifts from 1999 to 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baptist Health-University of Arkansas for Medical Sciences, North Little Rock, AR; 2Albalaq Applied University, Lockport, IL; 3Insight Hospital and Medical Center, Chicago, IL; 4Ascension Saint Joseph Hospital, Joliet, IL; 5Ascension Saint Joseph Medical Center, Joliet, IL; 6Baptist Health UAMS, North Little Rock, AR
Introduction: This study investigates liver disease mortality trends in the USA, encompassing various etiologies like viral infections, alcohol abuse, and metabolic disorders. The findings are expected to help with the targeted interventions and policies to reduce the burden of liver disease and improving public health outcomes nationwide.
Methods: We ultilized Centers for Disease Control and Prevention's (CDC) WONDER database, which provides comprehensive coverage of the entire US population. Leveraging the multiple cause of death database based on the International Classification of Diseases - 10th revision, we systematically identified all individuals who succumbed to liver disease (coded as K70-K76 as the underlying cause of death) from 1999 to 2020 in the United States. Subsequently, we stratified the data by race, irrespective of gender, and ethnic background. Age-adjusted mortality rates were then computed per 100,000 persons (PMP) and standardized to the US census data from 2000 to facilitate comparative analyses across different demographic groups and temporal periods.
Results: Across the interval spanning from 1999 to 2020, analysis of liver disease-related mortalities revealed a total of 975,492 fatalities, equating to an aggregate age-adjusted mortality rate of 132.1 per million population (PMP). Distinct variations were observed among racial groups, with Caucasians exhibiting a rate of 138 PMP, followed by African Americans at 109.2 PMP, Asian or Pacific Islanders at 50.1 PMP, and American Indian or Alaska Natives at 308.7 PMP. Overarching trends showcased a stark contrast in mortality shifts: a notable 49% escalation among Caucasians, rising from 121.2 PMP in 1999 to 180.5 PMP in 2020, juxtaposed with a significant 18% decline among African Americans, with rates plummeting from 139.5 PMP in 1999 to 114.1 PMP in 2020. Asian populations experienced a modest 9% increase, elevating from 52 PMP to 56.9 PMP over the studied period, while American Indian/Alaska Native communities encountered a pronounced 36% rise, escalating mortality rates from 304.6 PMP in 1999 to 414.4 PMP in 2020.
Discussion: During the last two decades, mortality surged for most, but not for African American population. Mortality was highest for Caucasians followed by American Indian/Alaska Native and Asian/Pacific Islander populations. Remarkably, African Americans had an 18% drop in liver disease deaths. Further exploration is needed to find the root cause for the drop in mortality in African American population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nosheen Hafeez indicated no relevant financial relationships.
Ehab Alkhawaldeh indicated no relevant financial relationships.
Sabri Elmansouri indicated no relevant financial relationships.
Bachar Hamad indicated no relevant financial relationships.
Sammy Hamad indicated no relevant financial relationships.
Mohamed Boshnaf indicated no relevant financial relationships.
Nosheen Hafeez, MD1, Ehab Alkhawaldeh, MD2, Sabri Elmansouri, MD, MPH3, Bachar Hamad, MD4, Sammy Hamad, DO5, Mohamed Boshnaf, MD, MPH6. P2964 - Liver Disease Mortality in the United States: Demographic Shifts from 1999 to 2020, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
