Monday Poster Session
Category: Liver
P2975 - Limitations of FIB-4 Score in Excluding Advanced Fibrosis in Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD)
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BB
Blake Bentley, MD
Wake Forest University School of Medicine
Winston-Salem, NC
Presenting Author(s)
Blake Bentley, MD1, Frank Ventura, MD1, Corey Obermmiller, 2, Mark Russo, MD, MPH3, Sean Rudnick, MD2
1Wake Forest University School of Medicine, Winston-Salem, NC; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC; 3Atrium Health, Charlotte, NC
Introduction: The obesity epidemic has seen a concomitant rise in associated conditions with approximately 5% of the U.S. population developing MASLD and up to 20% of patients with metabolic dysfunction-associated steatohepatitis (MASH) developing cirrhosis within 10 years. Noninvasive tests (NIT) are used to risk-stratify patients. These include liver stiffness measurement by vibration controlled transient elastography (LSM-VCTE) or ultrasound elastography (USe) and Fibrosis-4 Index (FIB4). Sequential use of FIB-4 followed by LSM-VCTE in population screening relies on the negative predictive value (NPV) of FIB-4 to exclude advanced fibrosis (AF). The aim of this study was to determine if low-risk FIB-4 scores fail to identify patients with MASLD and AF.
Methods: A retrospective EMR query based on ICD 9/10 codes for “NAFLD” (now MASLD) from 2012-2022 identified patients with results for NIT. This included serologic testing and elastography. Patients age >18 years with diagnosis of NAFLD were included. Patients with known cirrhosis or alternative etiologies of liver disease were excluded. Results were analyzed using descriptive statistics, fishers exact test, and analysis of variance.
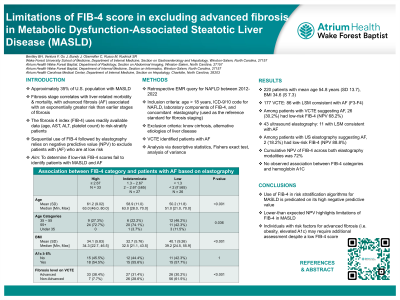
Results: 220 patients with a mean age of 54.8 years (SD 13.7) and BMI of 34.6 (SD 7.3) met inclusion criteria (177 VCTE, 43 USe). Of the 177 patients with VCTE, 86 had LSM consistent with advanced fibrosis (F3-F4), of whom 26 (30.2%) were characterized as low-risk based on FIB4 score (NPV 68.2%). Of 43 patients with USe, 11 has LSM consistent with AF, with 2 (18.2%) considered low risk based on FIB-4 (NPV 88.8%). Cumulative NPV with elastography was 72%. Among patients with AF on VCTE, statistical testing (Fishers exact test) revealed significant associations between FIB-4 category and factors such as BMI and age. There were no significant associations between FIB-4 categories and hemoglobinA1C.
Discussion: Use of the FIB-4 score in risk-stratification of patients with MASLD is predicated on its high negative predictive value (i.e. reliably excluding AF). The lower-than-expected NPV observed highlight limitations of FIB-4 in MASLD. Individuals with MASLD and risk factors for AF (i.e. obesity & diabetes/pre-diabetes) may require additional assessment despite low FIB-4 scores.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Blake Bentley, MD1, Frank Ventura, MD1, Corey Obermmiller, 2, Mark Russo, MD, MPH3, Sean Rudnick, MD2. P2975 - Limitations of FIB-4 Score in Excluding Advanced Fibrosis in Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wake Forest University School of Medicine, Winston-Salem, NC; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC; 3Atrium Health, Charlotte, NC
Introduction: The obesity epidemic has seen a concomitant rise in associated conditions with approximately 5% of the U.S. population developing MASLD and up to 20% of patients with metabolic dysfunction-associated steatohepatitis (MASH) developing cirrhosis within 10 years. Noninvasive tests (NIT) are used to risk-stratify patients. These include liver stiffness measurement by vibration controlled transient elastography (LSM-VCTE) or ultrasound elastography (USe) and Fibrosis-4 Index (FIB4). Sequential use of FIB-4 followed by LSM-VCTE in population screening relies on the negative predictive value (NPV) of FIB-4 to exclude advanced fibrosis (AF). The aim of this study was to determine if low-risk FIB-4 scores fail to identify patients with MASLD and AF.
Methods: A retrospective EMR query based on ICD 9/10 codes for “NAFLD” (now MASLD) from 2012-2022 identified patients with results for NIT. This included serologic testing and elastography. Patients age >18 years with diagnosis of NAFLD were included. Patients with known cirrhosis or alternative etiologies of liver disease were excluded. Results were analyzed using descriptive statistics, fishers exact test, and analysis of variance.
Results: 220 patients with a mean age of 54.8 years (SD 13.7) and BMI of 34.6 (SD 7.3) met inclusion criteria (177 VCTE, 43 USe). Of the 177 patients with VCTE, 86 had LSM consistent with advanced fibrosis (F3-F4), of whom 26 (30.2%) were characterized as low-risk based on FIB4 score (NPV 68.2%). Of 43 patients with USe, 11 has LSM consistent with AF, with 2 (18.2%) considered low risk based on FIB-4 (NPV 88.8%). Cumulative NPV with elastography was 72%. Among patients with AF on VCTE, statistical testing (Fishers exact test) revealed significant associations between FIB-4 category and factors such as BMI and age. There were no significant associations between FIB-4 categories and hemoglobinA1C.
Discussion: Use of the FIB-4 score in risk-stratification of patients with MASLD is predicated on its high negative predictive value (i.e. reliably excluding AF). The lower-than-expected NPV observed highlight limitations of FIB-4 in MASLD. Individuals with MASLD and risk factors for AF (i.e. obesity & diabetes/pre-diabetes) may require additional assessment despite low FIB-4 scores.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Blake Bentley indicated no relevant financial relationships.
Frank Ventura indicated no relevant financial relationships.
Corey Obermmiller indicated no relevant financial relationships.
Mark Russo indicated no relevant financial relationships.
Sean Rudnick indicated no relevant financial relationships.
Blake Bentley, MD1, Frank Ventura, MD1, Corey Obermmiller, 2, Mark Russo, MD, MPH3, Sean Rudnick, MD2. P2975 - Limitations of FIB-4 Score in Excluding Advanced Fibrosis in Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

