Monday Poster Session
Category: Liver
P2980 - Temporary Biliary Stenting During Liver Transplant to Prevent Anastomotic Biliary Strictures: A Single Center Retrospective Study
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rohan Rau, DO
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Rohan Rau, DO1, Wei Yan, MD1, Maria Lagarde Mussa, MD2
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Medical Center, Philadelphia, PA
Introduction: Complications after liver transplants have reduced as surgical technique, immunosuppression regimens and post-transplant monitoring have advanced. However, anastomotic biliary strictures (ABS) of the bile duct are a well-recognized complication of transplant and can lead to bile flow obstruction, cholangitis or choledocholithiasis. A novel surgical technique places a temporary biliary stent in the form of a pediatric feeding tube (PFT) during bile duct anastomotic reconstruction. The technique aims to prevent strictures by supporting the anastomotic site. This retrospective study evaluated the incidence of anastomotic biliary strictures in patients who received this novel technique.
Methods: This Institutional Review Board (IRB) approved study was based on the United Network of Organ Sharing (UNOS) list of transplanted patients at one center over a 7-year period. Only deceased-donor liver transplants (DDLT) who received the biliary stent in the form of a 5 or 6-French pediatric feeding tube were considered. Patients who did not undergo stenting, died in the first year, required re-transplantation, or lacked follow up were excluded. 402 patients were reviewed for ABS (primary outcome), post-operative complications and need for procedures. Strictures were sub-classified into clinically significant and those incidentally found on imaging. The overall incidence of ABS was compared against the largest meta-analysis of post-operative compilations. The difference was evaluated for statical significance.
Results: The technique reduced the incidence of anastomotic biliary strictures in a statistically significant manner. The incidence of ABS was 7.96%, compared to 12% in the largest meta-analysis on DDLT patients (p-value < 0.05). Furthermore, the incidence of clinically significant ABS was only 4.98% (p-value < 0.05) The incidence of cholangitis was 1.24% and the incidence of choledocholithiasis was 5.97%. ERCP for asymptomatic retained stents was required in 35 patients.
Discussion: This retrospective study evaluated 402 subjects and demonstrated that the technique had a statistically significant reduction in ABS. This suggests efficacy in preventing strictures, in turn preventing biliary complications and additional interventions. The low rate of complications suggests its safety. However, there is a need for ERCP to remove retained stents. Further subgroup analysis is required to help discern which patient features allow this procedure to garner the most success.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rohan Rau, DO1, Wei Yan, MD1, Maria Lagarde Mussa, MD2. P2980 - Temporary Biliary Stenting During Liver Transplant to Prevent Anastomotic Biliary Strictures: A Single Center Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Einstein Medical Center, Philadelphia, PA
Introduction: Complications after liver transplants have reduced as surgical technique, immunosuppression regimens and post-transplant monitoring have advanced. However, anastomotic biliary strictures (ABS) of the bile duct are a well-recognized complication of transplant and can lead to bile flow obstruction, cholangitis or choledocholithiasis. A novel surgical technique places a temporary biliary stent in the form of a pediatric feeding tube (PFT) during bile duct anastomotic reconstruction. The technique aims to prevent strictures by supporting the anastomotic site. This retrospective study evaluated the incidence of anastomotic biliary strictures in patients who received this novel technique.
Methods: This Institutional Review Board (IRB) approved study was based on the United Network of Organ Sharing (UNOS) list of transplanted patients at one center over a 7-year period. Only deceased-donor liver transplants (DDLT) who received the biliary stent in the form of a 5 or 6-French pediatric feeding tube were considered. Patients who did not undergo stenting, died in the first year, required re-transplantation, or lacked follow up were excluded. 402 patients were reviewed for ABS (primary outcome), post-operative complications and need for procedures. Strictures were sub-classified into clinically significant and those incidentally found on imaging. The overall incidence of ABS was compared against the largest meta-analysis of post-operative compilations. The difference was evaluated for statical significance.
Results: The technique reduced the incidence of anastomotic biliary strictures in a statistically significant manner. The incidence of ABS was 7.96%, compared to 12% in the largest meta-analysis on DDLT patients (p-value < 0.05). Furthermore, the incidence of clinically significant ABS was only 4.98% (p-value < 0.05) The incidence of cholangitis was 1.24% and the incidence of choledocholithiasis was 5.97%. ERCP for asymptomatic retained stents was required in 35 patients.
Discussion: This retrospective study evaluated 402 subjects and demonstrated that the technique had a statistically significant reduction in ABS. This suggests efficacy in preventing strictures, in turn preventing biliary complications and additional interventions. The low rate of complications suggests its safety. However, there is a need for ERCP to remove retained stents. Further subgroup analysis is required to help discern which patient features allow this procedure to garner the most success.
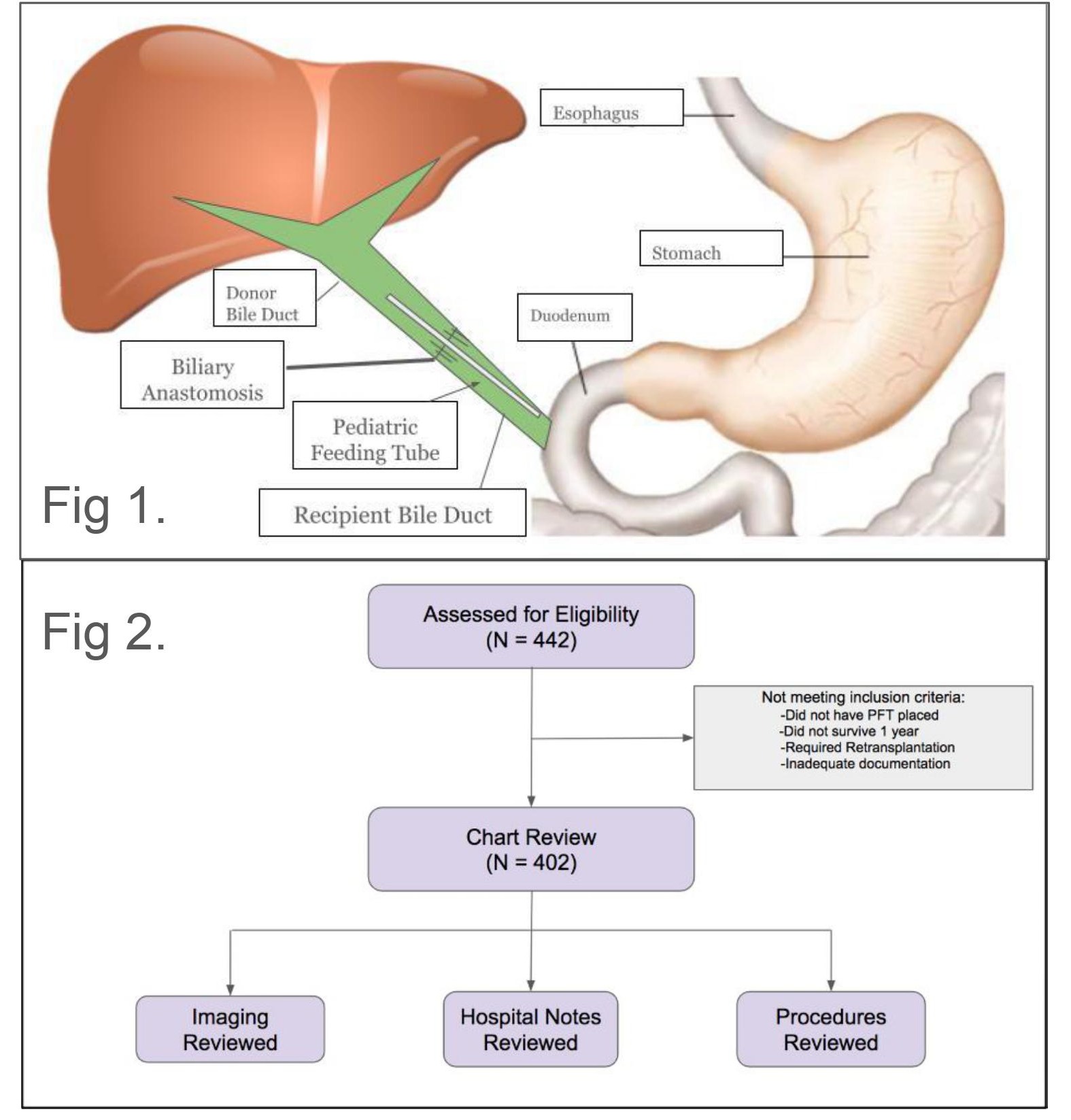
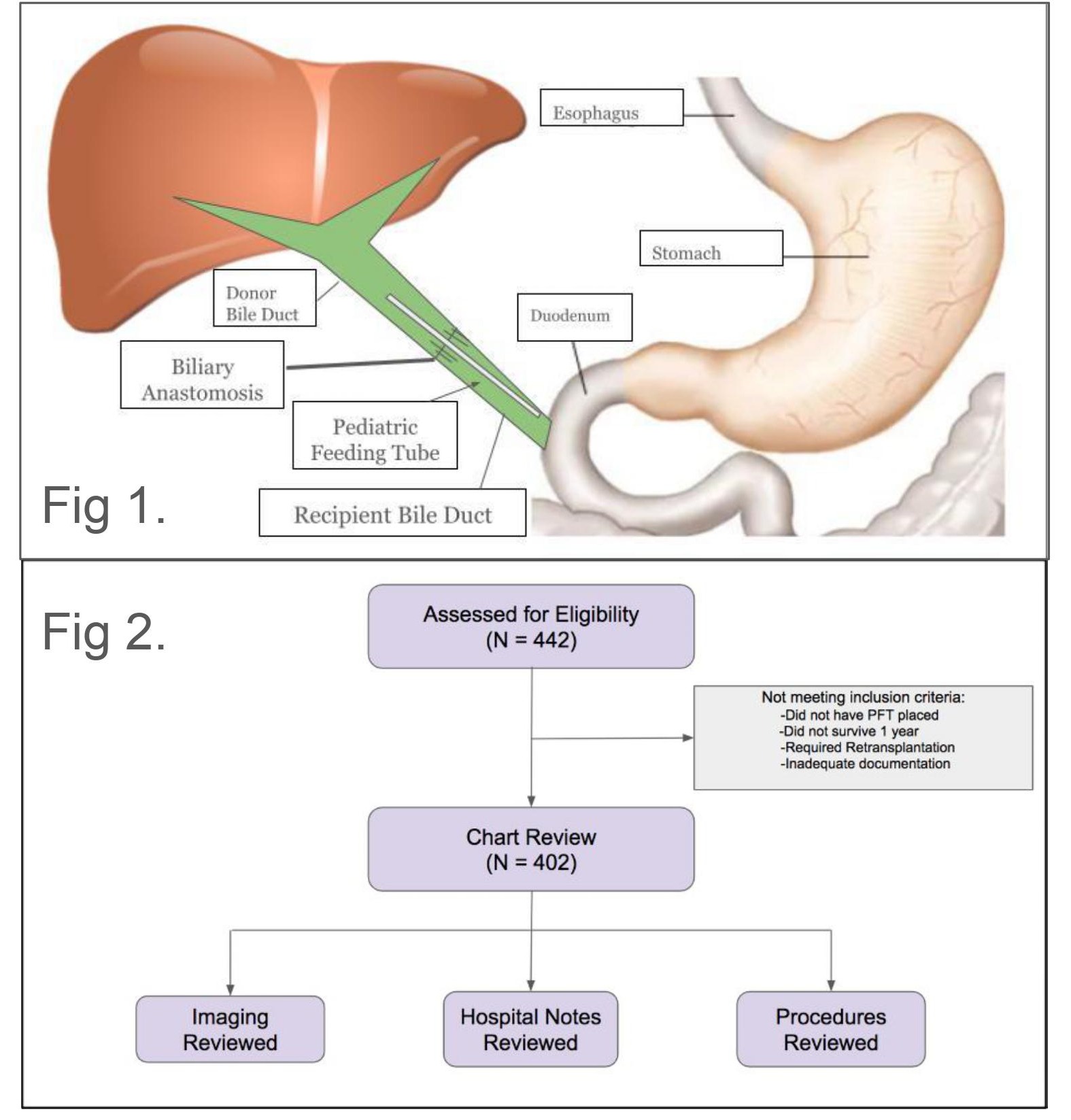
Figure: Figure 1: The temporary biliary stent is a pediatric feeding tube (PFT) placed at the site of the biliary anastomosis. Thus, it is able to support the biliary anastomosis, prevent against strictures and aid in biliary decompression
Figure 2: Methods pertaining to exclusion and inclusion criteria when selecting charts for analysis.
Figure 2: Methods pertaining to exclusion and inclusion criteria when selecting charts for analysis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rohan Rau indicated no relevant financial relationships.
Wei Yan indicated no relevant financial relationships.
Maria Lagarde Mussa indicated no relevant financial relationships.
Rohan Rau, DO1, Wei Yan, MD1, Maria Lagarde Mussa, MD2. P2980 - Temporary Biliary Stenting During Liver Transplant to Prevent Anastomotic Biliary Strictures: A Single Center Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
