Monday Poster Session
Category: Liver
P2981 - Hepatic Adenomatosis Transformation to Hepatocellular Carcinoma Secondary to Exogenous Testosterone Use
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Bibek Saha, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Bibek Saha, MD, Michael Leise, MD
Mayo Clinic, Rochester, MN
Introduction: Hepatocellular adenomas (HCAs) are an uncommon type of benign liver tumor and are typically diagnosed incidentally. HCAs are predominantly found in younger women who use estrogen containing medication including oral contraceptives but can be associated with androgenic steroid use. While rare, HCAs can undergo malignant transformation to hepatocellular carcinoma (HCC) especially in males with beta-catenin mutations. We present such a rare case in the context of chronic exogenous testosterone use.
Case Description/Methods: A 29-year-old male presented to the ED with a 5-day history of right upper quadrant (RUQ) abdominal pain, abdominal distension, nausea, chills and night sweats. He denied fatigue, weight loss, bowel habit changes and hematochezia. Family history revealed an uncle with hemochromatosis. He denied alcohol abuse but endorsed exogenous testosterone use for 10 years while weight training.
He was vitally stable. On physical exam, there was no jaundice, scleral icterus or cirrhotic skin findings. The abdomen was distended, with tenderness on palpation of the RUQ and epigastric regions.
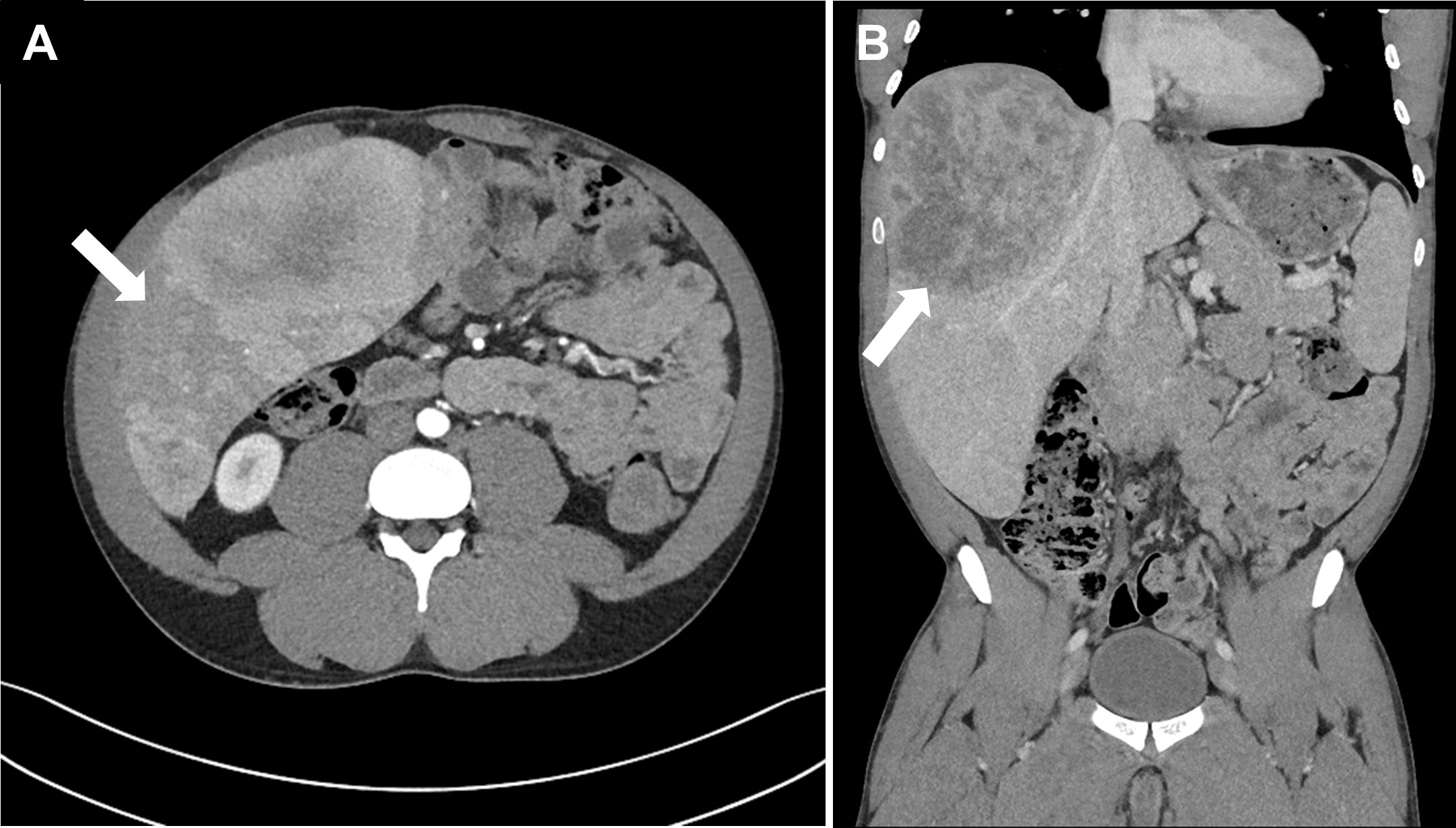
Labs revealed a hemoglobin of 12.2. Liver chemistries were significant for ALT and AST of 1102 and 487, respectively. AFP was 1.3 and INR was 1.2. Studies for hepatitis B and C were negative and ferritin was normal (32). Computed Tomography (CT) of the abdomen and pelvis showed innumerable ( >20) widespread liver masses concerning for primary malignancy or metastatic disease (Figure 1). Liver biopsy of a right lobe lesion with histopathology revealed a beta-catenin activated hepatic adenoma with early malignant transformation. He was dismissed with hepatology follow-up.
On staging imaging, there was no metastasis and the largest lesion measured 14.3x10.9cm. Given the lesion burden and bilobar involvement, surgical resection was not an option. Hepatic artery radioembolization was performed to prevent further HCC growth and he remains under surveillance awaiting liver transplantation.
Discussion: It is recommended that males with HCA, especially with beta-catenin mutations, undergo surgical resection given higher risk for HCC compared to females (47% versus 4%). However, given this patient already had HCC, liver transplantation is the treatment of choice. Taken together, while HCA is rare in men, clinicians should be aware of the higher risk for malignant transformation in this group given the rise of anabolic steroid use in young athletic males.
Disclosures:
Bibek Saha, MD, Michael Leise, MD. P2981 - Hepatic Adenomatosis Transformation to Hepatocellular Carcinoma Secondary to Exogenous Testosterone Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Hepatocellular adenomas (HCAs) are an uncommon type of benign liver tumor and are typically diagnosed incidentally. HCAs are predominantly found in younger women who use estrogen containing medication including oral contraceptives but can be associated with androgenic steroid use. While rare, HCAs can undergo malignant transformation to hepatocellular carcinoma (HCC) especially in males with beta-catenin mutations. We present such a rare case in the context of chronic exogenous testosterone use.
Case Description/Methods: A 29-year-old male presented to the ED with a 5-day history of right upper quadrant (RUQ) abdominal pain, abdominal distension, nausea, chills and night sweats. He denied fatigue, weight loss, bowel habit changes and hematochezia. Family history revealed an uncle with hemochromatosis. He denied alcohol abuse but endorsed exogenous testosterone use for 10 years while weight training.
He was vitally stable. On physical exam, there was no jaundice, scleral icterus or cirrhotic skin findings. The abdomen was distended, with tenderness on palpation of the RUQ and epigastric regions.
Labs revealed a hemoglobin of 12.2. Liver chemistries were significant for ALT and AST of 1102 and 487, respectively. AFP was 1.3 and INR was 1.2. Studies for hepatitis B and C were negative and ferritin was normal (32). Computed Tomography (CT) of the abdomen and pelvis showed innumerable ( >20) widespread liver masses concerning for primary malignancy or metastatic disease (Figure 1). Liver biopsy of a right lobe lesion with histopathology revealed a beta-catenin activated hepatic adenoma with early malignant transformation. He was dismissed with hepatology follow-up.
On staging imaging, there was no metastasis and the largest lesion measured 14.3x10.9cm. Given the lesion burden and bilobar involvement, surgical resection was not an option. Hepatic artery radioembolization was performed to prevent further HCC growth and he remains under surveillance awaiting liver transplantation.
Discussion: It is recommended that males with HCA, especially with beta-catenin mutations, undergo surgical resection given higher risk for HCC compared to females (47% versus 4%). However, given this patient already had HCC, liver transplantation is the treatment of choice. Taken together, while HCA is rare in men, clinicians should be aware of the higher risk for malignant transformation in this group given the rise of anabolic steroid use in young athletic males.
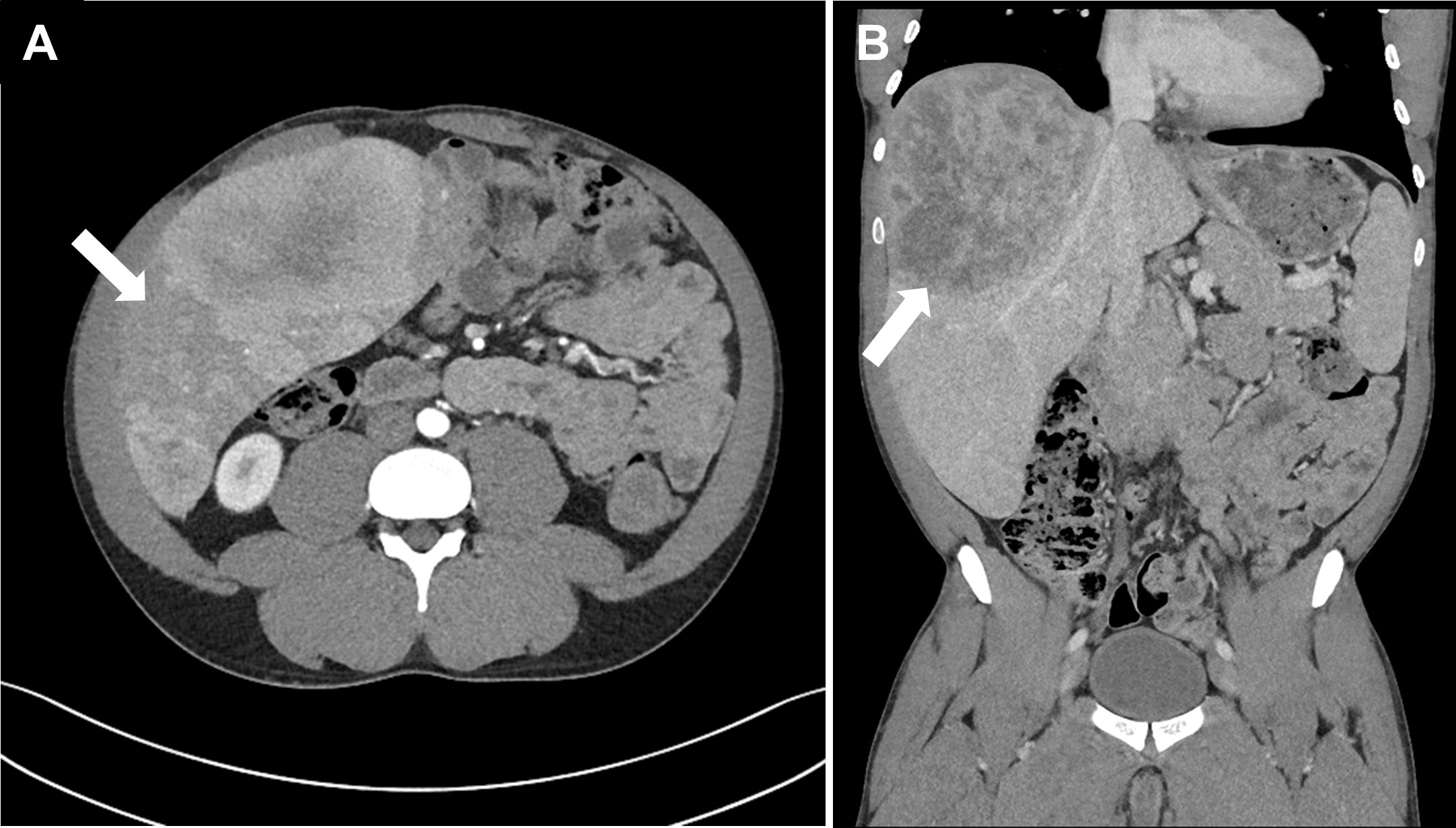
Figure: Figure 1. Computed Tomography of the abdomen and pelvis showing innumerable (>20) widespread liver masses (arrow) concerning for primary malignancy or metastatic disease. A) Axial view. B) Coronal view.
Disclosures:
Bibek Saha indicated no relevant financial relationships.
Michael Leise indicated no relevant financial relationships.
Bibek Saha, MD, Michael Leise, MD. P2981 - Hepatic Adenomatosis Transformation to Hepatocellular Carcinoma Secondary to Exogenous Testosterone Use, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
